I know everyone is doing this, but here are my reflections after 2 wks in #ICU w/ #COVID19. Also includes lessons from our outstanding collaboration w/ #RapidResponseTeam
(1/12)
(1/12)
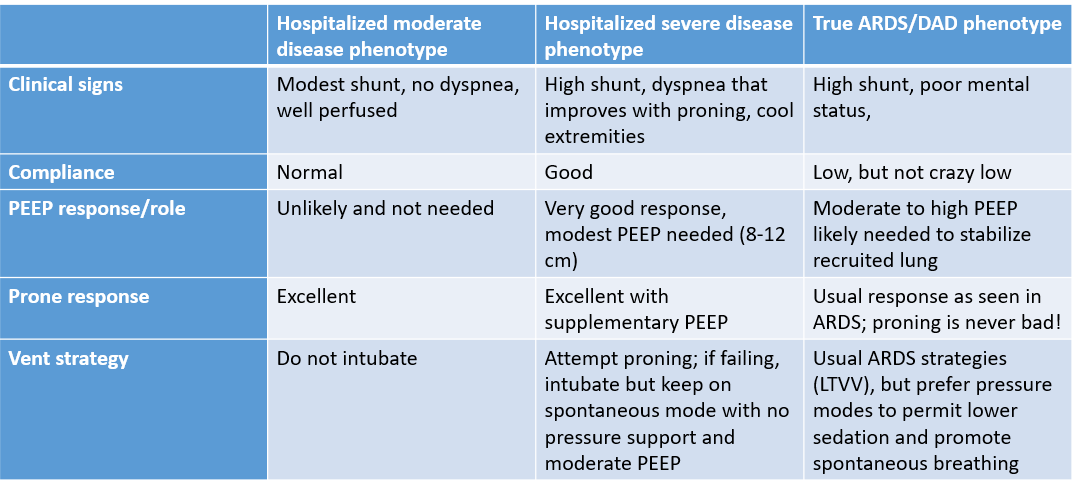
Much discussion on clinical phenotypes, but like any disease, #COVID19 is a spectrum. Here are 3 big phenotypes I saw
(2/2)
(2/2)
I’m more worried about running out of #intensivist, #RespiratoryTherapists, etc than running out of #ventilators. Given wide spectrum of disease, true expertise in mech ventilation needed. No 1-size-fits-all approach here
#COVID19 #VentilatorShortage
(3/12)
#COVID19 #VentilatorShortage
(3/12)
Nothing beats proning. I know many centers now doing this, reporting good results on #medtwitter.
Even post-pandemic, I’m going to try awake prone on HHHFNC for all pts w/ hypoxemic RF & acceptable WOB. Amazing strategy
(4/12)
Even post-pandemic, I’m going to try awake prone on HHHFNC for all pts w/ hypoxemic RF & acceptable WOB. Amazing strategy
(4/12)
Still not sure what to make of SpO2 vs SaO2 vs PaO2 discordances & not sure what to do clinically w/ it. Settled on checking SvO2 when in doubt to look at end-organ O2 delivery (but obviously major limitations there)
(5/12)
(5/12)
Also not sure what to do about #anticoagulation. Basically, I started empiric tx when discordance between minute ventilation & degree of hypoxemia in context of rising D-dimer
(6/12)
(6/12)
Proactive about diuresis from day 1, kept fluid balance net even. Challenges the idea of diuresing someone into AKI. AKI developing only in pts w/ high inflammatory state which is likely due to multiple mechanisms & never related to being in net fluid balance
(7/12)
(7/12)
Not sure what to do w/ CRP, ferritin, LDH, D-dimer, neutrophil-to-lymphocyte ratio, etc. These markers always correlate w/ clinical picture. Look at the patient, clinical trajectory, organ failures, etc
(8/12)
(8/12)
Very little #POCUS use (maybe 3 pts), and when I did, just to look at heart (RV esp), not lungs
Always #ccecho findings predicted by physical findings & context. Did not change mgmt.
Really doubt lung #POCUS has much role in ICU #COVID19 pts & would not #echofirst
(9/12)
Always #ccecho findings predicted by physical findings & context. Did not change mgmt.
Really doubt lung #POCUS has much role in ICU #COVID19 pts & would not #echofirst
(9/12)
Nurses & RTs have incredible resolve & still are most underappreciate resource (by general public) in #ICU care
Differences in outcomes for pts will ultimately be related to adequacy & quality of RN care, RT, #rapidresponse systems, not medications, # of vents, etc
(10/12)
Differences in outcomes for pts will ultimately be related to adequacy & quality of RN care, RT, #rapidresponse systems, not medications, # of vents, etc
(10/12)
Like any critical illness, encephalopathy & delirium are huge issues in older pts, likely to be a major contributor to why many older pts succumb to #COVID19
Difficult to manage #delirium when no visitors, pts kept prone, etc
(11/12)
Difficult to manage #delirium when no visitors, pts kept prone, etc
(11/12)
Finally, emotional toll even higher than usual in ICU… Families, patients, everyone
I cannot imagine struggles of families in these times, probably very difficult to trust #healthcare team when you can& #39;t see it firsthand
Expect a big #ICU #burnout wave post #COVID19
(12/12)
I cannot imagine struggles of families in these times, probably very difficult to trust #healthcare team when you can& #39;t see it firsthand
Expect a big #ICU #burnout wave post #COVID19
(12/12)
Oh, and now that I get a break from #COVID19 and #ICU, I finally get all the fuss over #TigerKingNetflix  https://abs.twimg.com/hashflags... draggable="false" alt="">
https://abs.twimg.com/hashflags... draggable="false" alt="">

 Read on Twitter
Read on Twitter