COVID DEATHS IN MALAYSIA
Adjunct Prof Dato’ Dr Musa Mohd Nordin, Consultant Paediatrician & Neonatologist, KPJ-DSH
Prof Dato’ Dr Azizi Omar, Consultant Paediatrician & Paediatric Respiratory Physician & Clinical Epidemiologist. KPJ-DSH
Muhamad Ariff Sodri BA Financial Analyst
Adjunct Prof Dato’ Dr Musa Mohd Nordin, Consultant Paediatrician & Neonatologist, KPJ-DSH
Prof Dato’ Dr Azizi Omar, Consultant Paediatrician & Paediatric Respiratory Physician & Clinical Epidemiologist. KPJ-DSH
Muhamad Ariff Sodri BA Financial Analyst
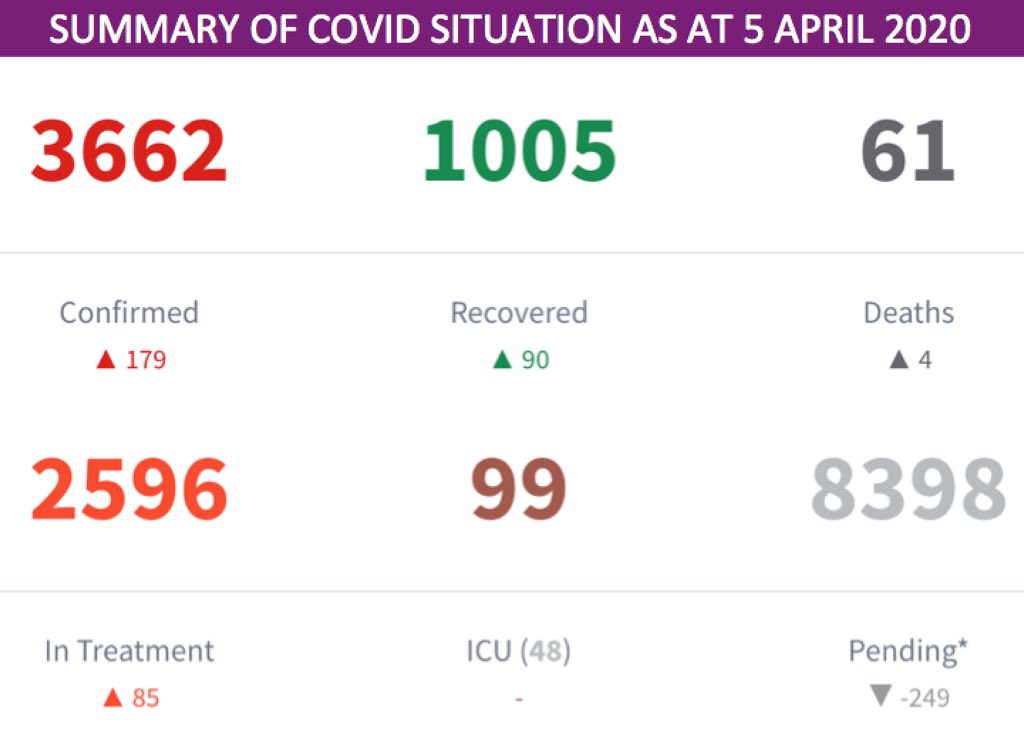
We painstakingly compiled the raw data of 61 COVID deaths.
The data are only what is known on some characteristics of those who died (N = 61)
There are no data on those who survived.
The total no of COVID cases as of 05.04.20 = 3662
No info known about 3601 cases.
The data are only what is known on some characteristics of those who died (N = 61)
There are no data on those who survived.
The total no of COVID cases as of 05.04.20 = 3662
No info known about 3601 cases.
As researchers our interests (objectives) are:
1. Descriptive features of those who died
2. Predictive (prognostic) factors for survival/death
3. Predictive (prognostic ) factors for severe disease (grade 4-5)
4. Comparative effectiveness of therapeutic interventions.
1. Descriptive features of those who died
2. Predictive (prognostic) factors for survival/death
3. Predictive (prognostic ) factors for severe disease (grade 4-5)
4. Comparative effectiveness of therapeutic interventions.
5. Cost effectiveness of interventional/therapeutic modalities
6. Qualitative (Soc Sci) enquiry of policy/decision making/strategic thinking as the pandemic unfolded.
From the data we have, we can mainly do no. 1, with occasional statistical comparison using known denominators.
6. Qualitative (Soc Sci) enquiry of policy/decision making/strategic thinking as the pandemic unfolded.
From the data we have, we can mainly do no. 1, with occasional statistical comparison using known denominators.
We can only describe what we see fr a case series of 61 deaths.
No sophisticated statistical analysis is possible at this stage. N =61 is statistically small but for a descriptive analysis it should do
China has > 3000 deaths, thus a robust descriptive and complex stats analysis.
No sophisticated statistical analysis is possible at this stage. N =61 is statistically small but for a descriptive analysis it should do
China has > 3000 deaths, thus a robust descriptive and complex stats analysis.
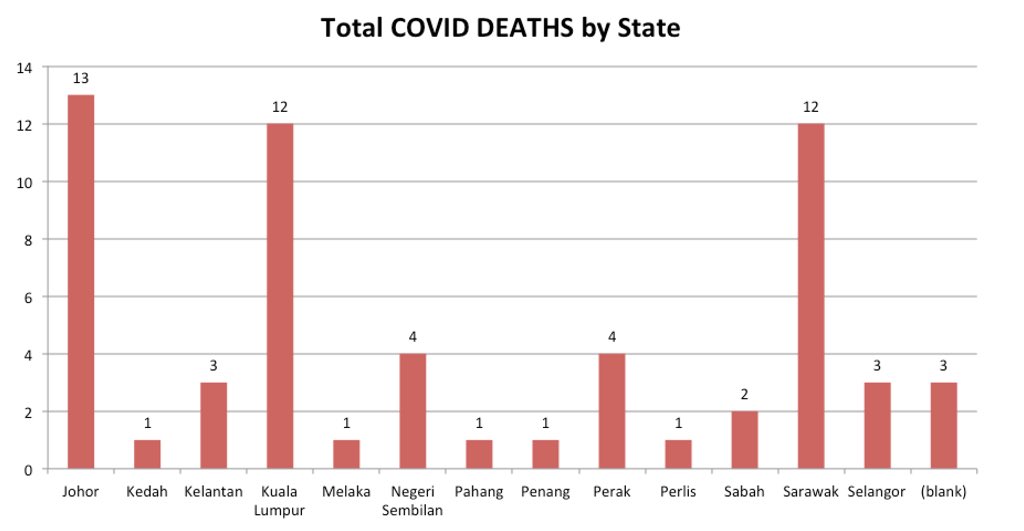
COVID Deaths by states
Klang Valley- 15 deaths (24.6%)
Johor- 13 deaths (21.3%)
Sarawak- 12 deaths (19.7%)
Klang Valley- 15 deaths (24.6%)
Johor- 13 deaths (21.3%)
Sarawak- 12 deaths (19.7%)
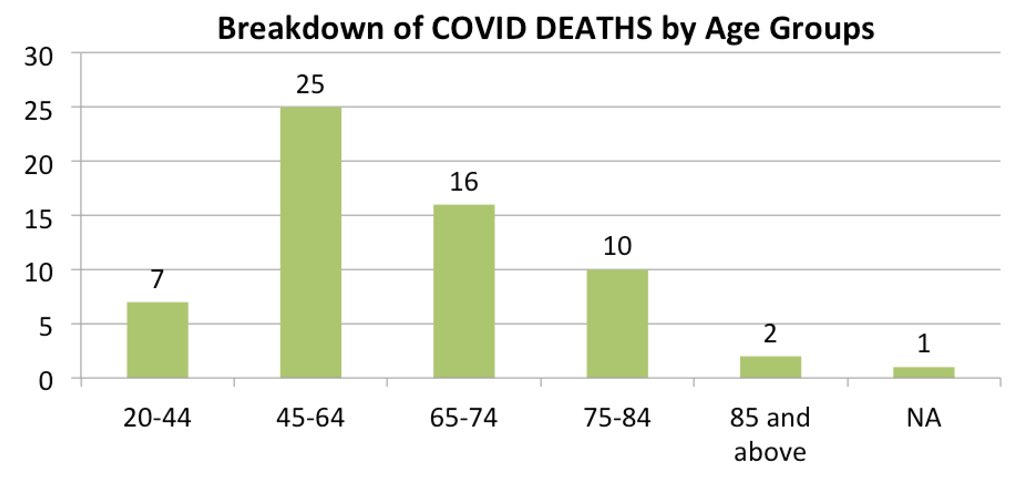
26 deaths (45.9%) in those >65 years old.
25 deaths (40.9%) in 45-65 age group
7 deaths (11.5%) in 20-44 age group
But conclusion of older age as risk for death can only be robust if we can compare CFR between older & younger age gp. Probably not possible to do with data we have.
25 deaths (40.9%) in 45-65 age group
7 deaths (11.5%) in 20-44 age group
But conclusion of older age as risk for death can only be robust if we can compare CFR between older & younger age gp. Probably not possible to do with data we have.
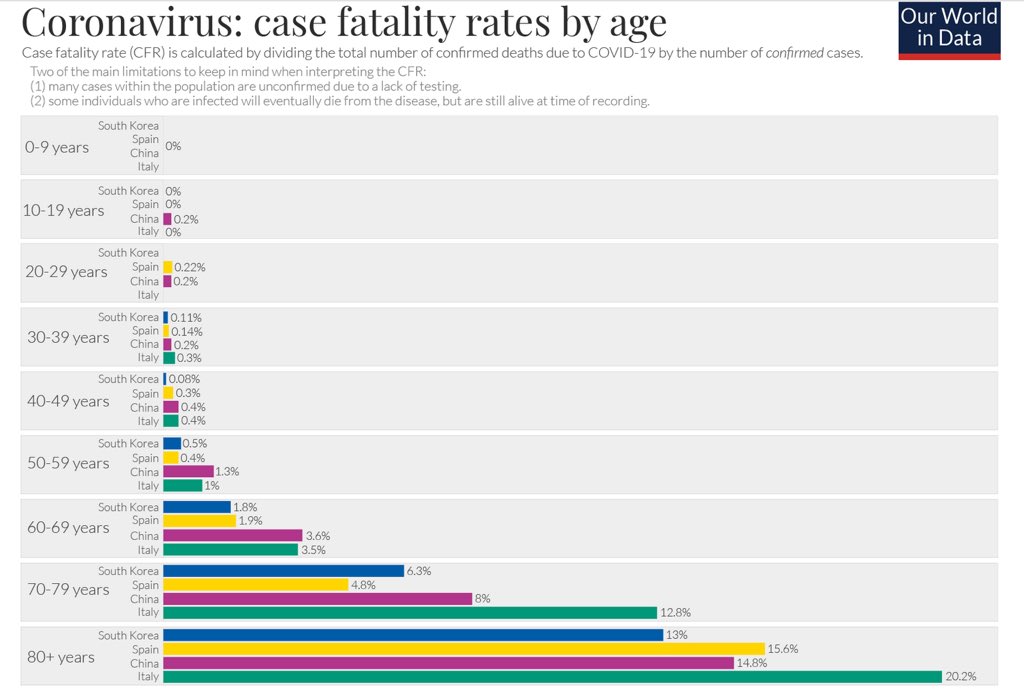
Compare this with data from the Chinese CDC (till 17 Feb 2020).
For COVID, the elderly are at greatest risk of dying due to their advanced age and the presence of co-morbidities
For COVID, the elderly are at greatest risk of dying due to their advanced age and the presence of co-morbidities
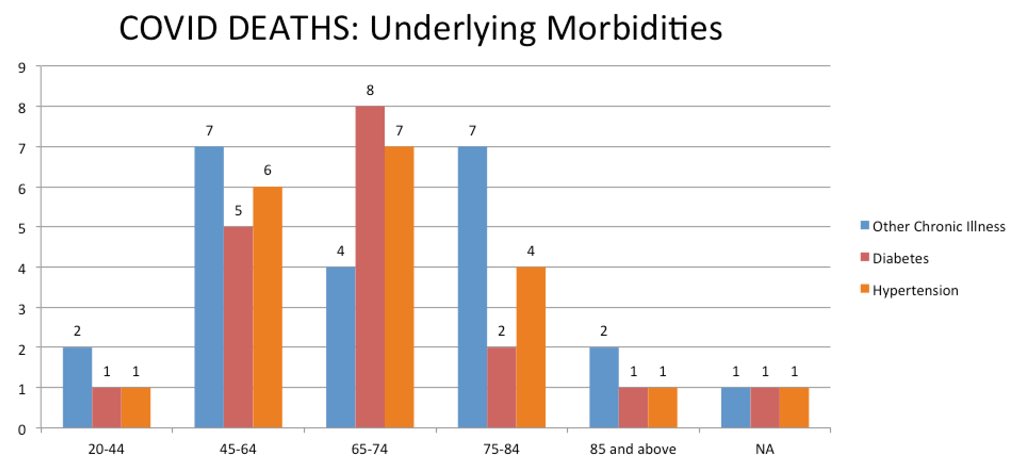
23/61 (37.7%) had other chronic illness
20/61(32.7%) had hypertensionu2028
18/61 (29.5%) had diabetesu2028
7/61 (11.5%) had 3 co-morbidities
10/61 (16.4%) had 2 co-morbidities
37/61 (60.6%) had at least 1 co-morbidity
20/61(32.7%) had hypertensionu2028
18/61 (29.5%) had diabetesu2028
7/61 (11.5%) had 3 co-morbidities
10/61 (16.4%) had 2 co-morbidities
37/61 (60.6%) had at least 1 co-morbidity
A better presentation if the data is available is the percentage of those with risk factors die - ie CFR stratified by comorbidities.
Unfortunately we do not have the denominator to calculate the CFR.
Unfortunately we do not have the denominator to calculate the CFR.
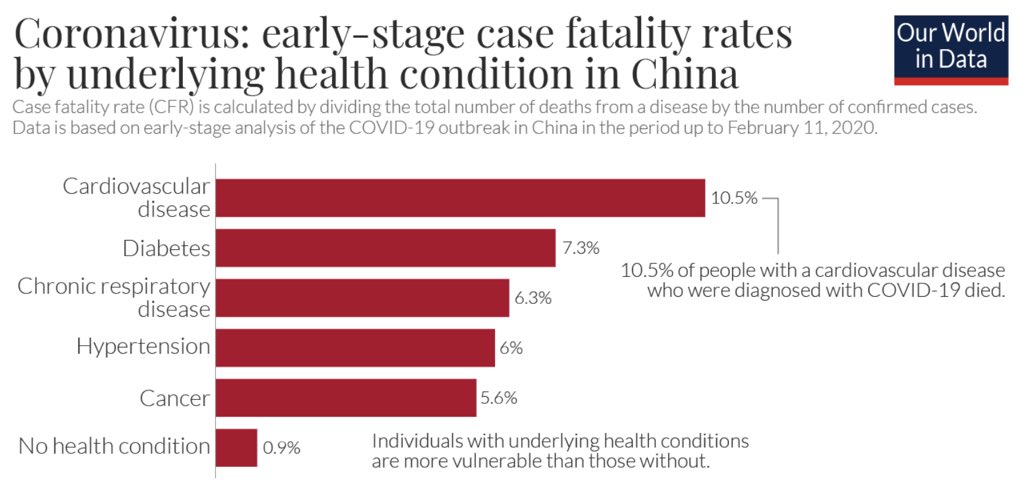
The Chinese CDC illustrated that those with underlying health condition is at much higher risk
10.5% persons with heart problems and who had COVID died.
Diabetes-7%
Chronic Lung Disease- 6%
Cancer- 5.6%
CFR was 0.9% for those without a pre-existing health condition
10.5% persons with heart problems and who had COVID died.
Diabetes-7%
Chronic Lung Disease- 6%
Cancer- 5.6%
CFR was 0.9% for those without a pre-existing health condition
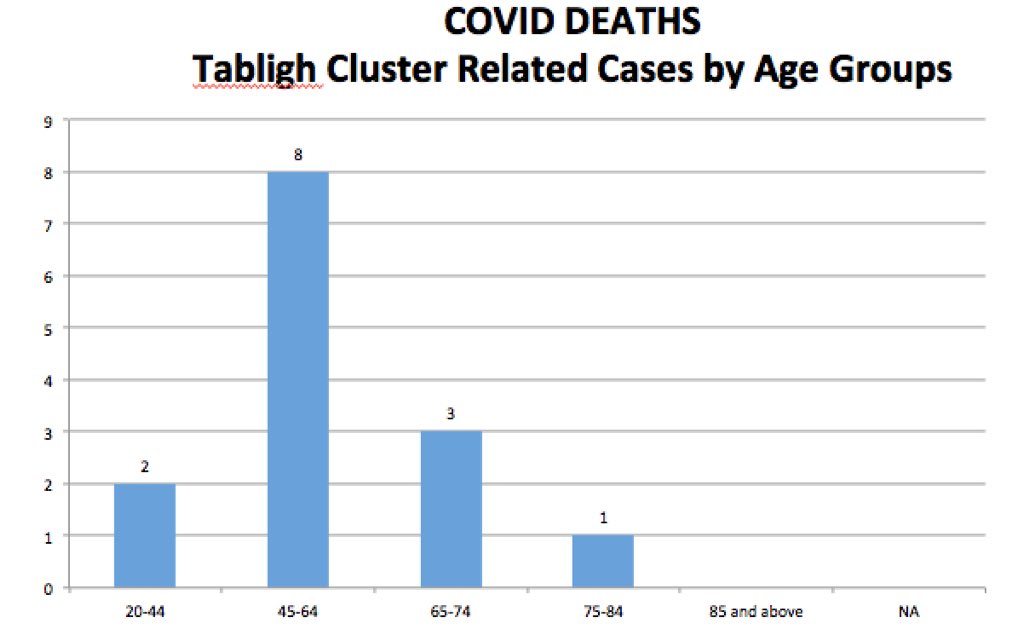
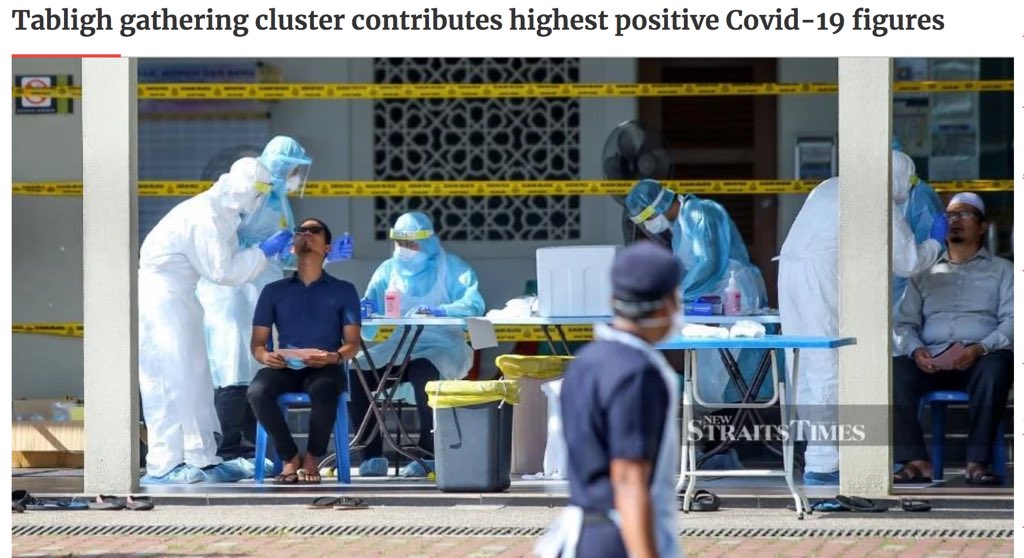
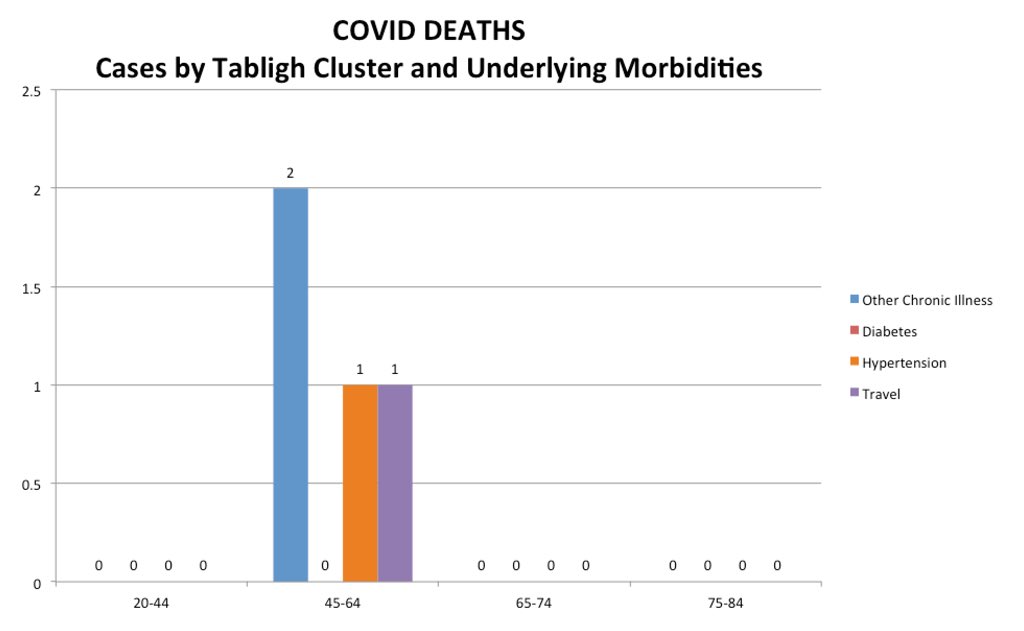
Tabligh cluster contributed 14/61 (23%) of deaths.
One can only suggest that the COVID viral load among the Tabligh participants was high.
Due to the extreme proximity ie overcrowding in a small zone, poor ventilation, sleeping, listening to lectures, eating ...
One can only suggest that the COVID viral load among the Tabligh participants was high.
Due to the extreme proximity ie overcrowding in a small zone, poor ventilation, sleeping, listening to lectures, eating ...
praying together in close proximity and the culture of handshaking, hugging, kissing as a show of love and brotherhood among the Tabligh fraternity 1545/3483 cases (44.36%) were linked to the Ijtima’ Tabligh at Sri Petaling (4/4/2020) on 28/2-1/3
If the total Tabligh positive cases are known a crude non-robust analysis can be made comparing Tabligh CFR vs CFR others.
MOH has detected five generations of positive COVID cases that were ah linked to the tabligh gathering.
711 cases had infected their families
MOH has detected five generations of positive COVID cases that were ah linked to the tabligh gathering.
711 cases had infected their families
The Tabligh cluster did not have any significant underlying co-morbidities to make them more vulnerable health wise.
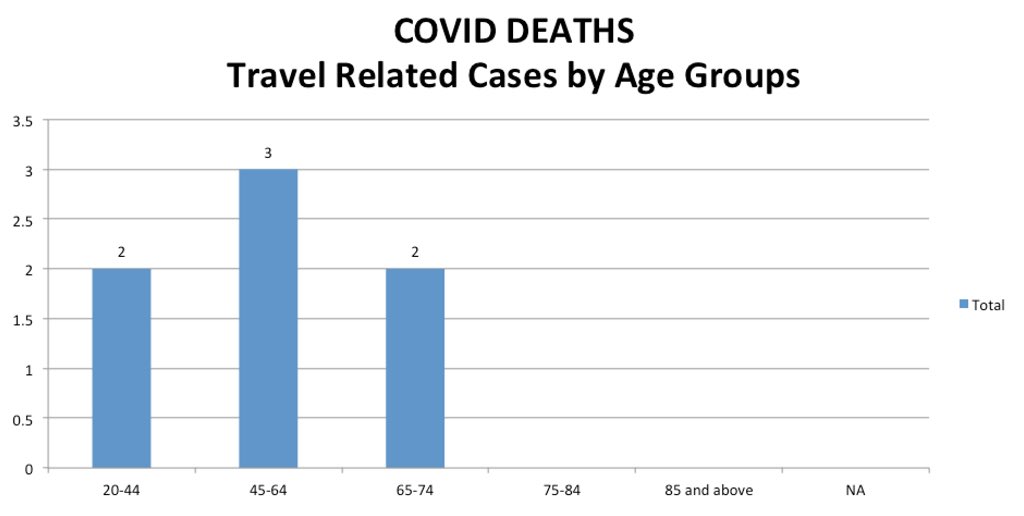
Only 7/61 (11.4%) had a travel history.
Travel history as a risk factor of COVID Deaths appears not as important at this stage ...to be continued
Travel history as a risk factor of COVID Deaths appears not as important at this stage ...to be continued
@threadreaderapp unroll

 Read on Twitter
Read on Twitter