As a GP-Anesthetist, I’m called to put people on life support measures like ventilators.
As a palliative care doctor, I keep people comfortable during the last phase of life, dying, whether that takes days or years.
Both skills are being put to the test in #COVID19Pandemic.
As a palliative care doctor, I keep people comfortable during the last phase of life, dying, whether that takes days or years.
Both skills are being put to the test in #COVID19Pandemic.
We have watched the #COVID19Pandemic bring hospital systems around the world to their knees.
We know that even in our healthcare system, we have nowhere near the resources we need. We do not have enough beds. We do not have enough doctors and nurses. We do not have enough vents.
We know that even in our healthcare system, we have nowhere near the resources we need. We do not have enough beds. We do not have enough doctors and nurses. We do not have enough vents.
In some instances, we can stretch — doctors for, example, know that they will be called on to practice beyond their usual scope.
They will do what needs doing, and they will answer the call of duty in the #COVID19Pandemic.
They will do what needs doing, and they will answer the call of duty in the #COVID19Pandemic.
But here it is:
We do not have enough beds to hospitalize everyone.
We do not have enough vents to put everyone on life support.
We do not have enough to do everything for everyone.
That is the reality every single healthcare system including ours is facing with #Covid19.
We do not have enough beds to hospitalize everyone.
We do not have enough vents to put everyone on life support.
We do not have enough to do everything for everyone.
That is the reality every single healthcare system including ours is facing with #Covid19.
Most people who get #COVID19 will recover on their own.
20% will need hospitalization.
5% will need life support.
The ones who have serious disease will include
*some young, healthy people
*some young people with other serious health issues
*many, many frail, older people.
20% will need hospitalization.
5% will need life support.
The ones who have serious disease will include
*some young, healthy people
*some young people with other serious health issues
*many, many frail, older people.
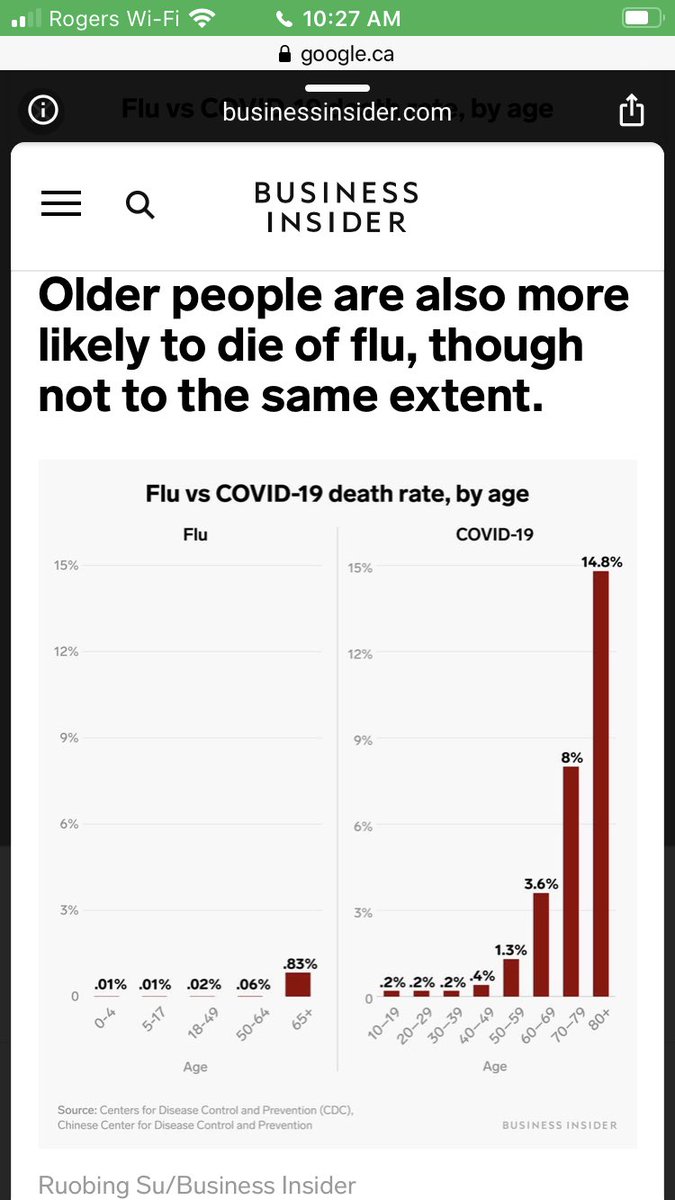
Elderly people with or without dementia, heart disease, kidney failure, lung disease, cancer and so on face a high mortality rate with #COVID19.
Isolation is the only way to protect them. When that doesn’t work, the best treatment for them is supportive care.
There is no cure.
Isolation is the only way to protect them. When that doesn’t work, the best treatment for them is supportive care.
There is no cure.
Putting elderly people on a ventilator or life support does not help. Once you go on a ventilator because of #Covid_19, you have an up to 86% chance of dying.
That means dying alone and unconscious after weeks of breathing through a life support machine. https://www.npr.org/sections/health-shots/2020/04/02/826105278/ventilators-are-no-panacea-for-critically-ill-covid-19-patients">https://www.npr.org/sections/...
That means dying alone and unconscious after weeks of breathing through a life support machine. https://www.npr.org/sections/health-shots/2020/04/02/826105278/ventilators-are-no-panacea-for-critically-ill-covid-19-patients">https://www.npr.org/sections/...
We all die. It’s scary yet true. But a good death matters as much as a good life.
Dying on a machine is not how I want to die. Ever. Most doctors I know agree.
That’s why #palliativecare matters.
A #GoodDeath matters, especially now.
Via @TorontoStar: https://www.thestar.com/news/gta/2020/04/05/the-dying-should-not-be-abandoned-palliative-caregivers-brace-for-heart-wrenching-scenarios-ahead-of-covid-surge.html">https://www.thestar.com/news/gta/...
Dying on a machine is not how I want to die. Ever. Most doctors I know agree.
That’s why #palliativecare matters.
A #GoodDeath matters, especially now.
Via @TorontoStar: https://www.thestar.com/news/gta/2020/04/05/the-dying-should-not-be-abandoned-palliative-caregivers-brace-for-heart-wrenching-scenarios-ahead-of-covid-surge.html">https://www.thestar.com/news/gta/...
A #GoodDeath in #Covid_19 means:
* medications to treat pain and shortness of breath — “air hunger.”
* your family & friends can tell you they love you.
* your family & friends can say goodbye.
Think about it. Talk about it with your loved ones. This is the time.
* medications to treat pain and shortness of breath — “air hunger.”
* your family & friends can tell you they love you.
* your family & friends can say goodbye.
Think about it. Talk about it with your loved ones. This is the time.
I saw this article by @globalnews:
https://globalnews.ca/news/6779888/coronavirus-ontario-long-term-care-homes-preparing-families-for-the-worst/
It">https://globalnews.ca/news/6779... broke my heart. Because as a society, we should have been talking about a #GoodDeath and #PalliativeCare long before the #COVID19Pandemic.
The government must be honest with its people. It’s time.
#ONpoli #CdnPoli
https://globalnews.ca/news/6779888/coronavirus-ontario-long-term-care-homes-preparing-families-for-the-worst/
It">https://globalnews.ca/news/6779... broke my heart. Because as a society, we should have been talking about a #GoodDeath and #PalliativeCare long before the #COVID19Pandemic.
The government must be honest with its people. It’s time.
#ONpoli #CdnPoli

 Read on Twitter
Read on Twitter