A thread on DNACPR (Do Not Attempt Cardiopulmonary Resuscitation). (1/29)
My credentials are these:
I& #39;ve been a doctor since 2012. I am a specialist registrar in Acute Medicine, and like most senior medical trainees I hold a certification in Advanced Life Support which qualifies me to lead a cardiac arrest team. (2/29)
I& #39;ve been a doctor since 2012. I am a specialist registrar in Acute Medicine, and like most senior medical trainees I hold a certification in Advanced Life Support which qualifies me to lead a cardiac arrest team. (2/29)
My credentials are also these:
I am the 34 year old orphan of two parents who both died far too young, and who both died with completely appropriate DNACPR forms in place. (3/29)
I am the 34 year old orphan of two parents who both died far too young, and who both died with completely appropriate DNACPR forms in place. (3/29)
This weekend, I& #39;m seeing a lot of discussion on issues around DNACPR. I& #39;m seeing a lot of journalistic misinformation, misunderstanding, crossed wires and difficult communication, and a lot of understandable distress. (4/29)
CPR is the term we use for chest compressions and electric shocks to the heart. It is a treatment for a person who has had a cardiac arrest. This means that their heart has stopped beating – in other words, when they have already died. (5/29)
DNACPR does not mean "euthanise". (6/29)
DNACPR does not mean "do not attempt – " :
- hospital admission
- fluids
- antibiotics
- oxygen
- treatment in an intensive care or high dependency unit (7/29)
- hospital admission
- fluids
- antibiotics
- oxygen
- treatment in an intensive care or high dependency unit (7/29)
There are also conversations about whether people would benefit from these treatments, and some people would not and those are reasonable conversations to have. But a DNACPR form does not prevent any treatment other than chest compression and electric shocks. (8/29)
If a person does not have a DNACPR form in place and they have a cardiac arrest in hospital, the first responder will start chest compressions and put out an emergency call to summon the cardiac arrest team. (9/29)
The family will be removed from the person& #39;s room. (10/29)
A team of doctors and nurses will descend. The person will get chest compressions, which will break their ribs. They will get various tubes shoved down their throat. They will be given special drugs to try to help restart the heart. (11/29)
In all circumstances, its success rate is small. (12/29)
In a proportion of people, a cardiac arrest is caused by an acutely reversible problem such as a heart attack, hypothermia, a salt imbalance, major trauma, or a poison. (13/29)
CPR pumps the heart artificially, keeping oxygen circulating to vital organs. In people with acutely reversible problems like this, it might buy us some time to fix the acute problem and we would probably say that that chance is worth the trauma we cause by doing it. (14/29)
But it still fails for more people than it works for.
And for people who do not have an acutely reversible problem, it will fail.
And for people who are elderly or frail, it will fail anyway. (15/29)
And for people who do not have an acutely reversible problem, it will fail.
And for people who are elderly or frail, it will fail anyway. (15/29)
In the majority of people, a cardiac arrest is the end stage of what we might otherwise call Ordinary Dying. (16/29)
And for people whIn these circumstances, CPR would not work. No doctor is obliged to provide a treatment that would not work. It is a medical decision. It is not the decision of the person, or their relative. They are not asked to sign the DNACPR form. (17/29)
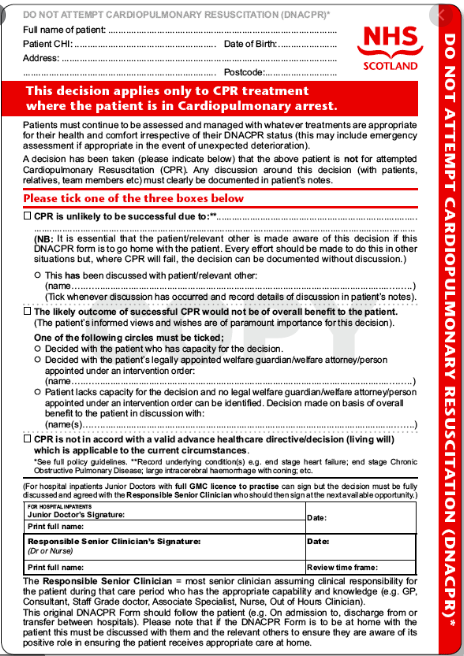
For illustration, this is a DNACPR form in Scotland. It is substantively identical throughout the rest of the UK. (18/29)
The law around DNACPR has not changed since 2015 (Tracey vs Cambridge University Hospital NHS FT), which led to greater transparency, obligating CPR decisions to be discussed and communicated.
This sometimes leads to the perception that people are being "asked to sign". (19/29)
This sometimes leads to the perception that people are being "asked to sign". (19/29)
There has been no change in the law around DNACPR in the emergency powers within the Coronavirus Act. (20/29)
In irreversible cardiac arrest, or Ordinary Dying, a DNACPR form allows us to say that when a person& #39;s heart stops beating this means that they have died. (21/29)
They will be protected from the indignity and brutality of a cardiac arrest team& #39;s arrival, and their family will be able to stay with them.
Even in the age of pandemic, most hospitals have tried to make provision for a relative to be with a person near the end of life. (22/29)
Even in the age of pandemic, most hospitals have tried to make provision for a relative to be with a person near the end of life. (22/29)
My impression is that some of this has been very badly communicated, and that people have understandably believed that these things are happening because of COVID19. (23/29)
COVID19 has increased the urgency of making sure that people have appropriate protections in place against inappropriate treatments. We have needed to be more willing to have the scary and uncomfortable conversation, when in the past we might have avoided them. (24/29)
The truth is that these are conversations that should already have been taking place, with or without a global medical emergency to focus our minds. (25/29)
I am aware that there are cases where the conversation has been had very badly, or when the conversation has been had by text messages or letters, and that this has caused enormous distress. For this, I am sorry. (26/29)
We are not God, and we cannot prevent all death, and there are times when the best and kindest thing we can do is to recognise that and to do what we can to make it a good death. (27/29)
For more and better reading, I recommend this part of @DrLindaDykes& #39;s website: https://www.lindadykes.org/havetheconversation">https://www.lindadykes.org/havetheco... (28/29)
And I recommend everything written by @drkathrynmannix, but especially her book "With The End In Mind". (29/29)

 Read on Twitter
Read on Twitter