0/ Buongiorno, #medtwitter! We bring to you a #tweetorial on ventilator management for all those folks who don’t normally manage ARDS who have stepped up to help in this pandemic.
All credit goes to @AvrahamCooperMD; the following tweetorial is his brainchild. Thanks, Avi!
All credit goes to @AvrahamCooperMD; the following tweetorial is his brainchild. Thanks, Avi!
1/ Many clinicians are being/will be called to manage ARDS on the ventilator.
Imagine that your patient has just been intubated. Let& #39;s walk through the steps of vent mgmt 101:
- Initial housekeeping
- Basic vent management decisions in ARDS
- Management of refractory hypoxemia
Imagine that your patient has just been intubated. Let& #39;s walk through the steps of vent mgmt 101:
- Initial housekeeping
- Basic vent management decisions in ARDS
- Management of refractory hypoxemia
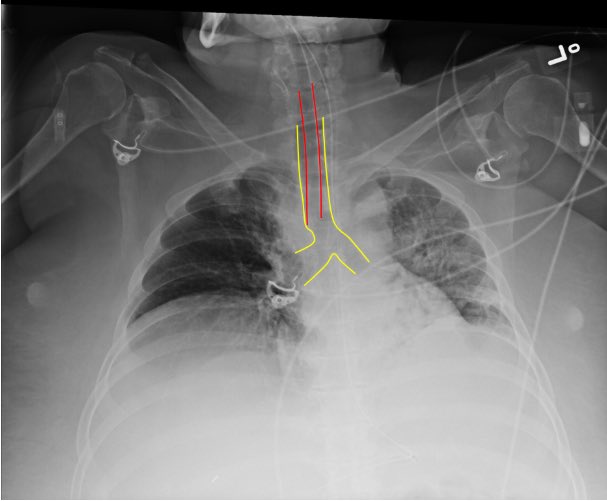
2/ First, confirm endotracheal tube position:
- Did capnography confirm tracheal placement?
- Are breath sounds bilateral?
- Is the tube placed appropriately on CXR? (typically 2-5 cm from carina)
Pic from SAEM https://bit.ly/3bJrTpa ">https://bit.ly/3bJrTpa&q...
- Did capnography confirm tracheal placement?
- Are breath sounds bilateral?
- Is the tube placed appropriately on CXR? (typically 2-5 cm from carina)
Pic from SAEM https://bit.ly/3bJrTpa ">https://bit.ly/3bJrTpa&q...
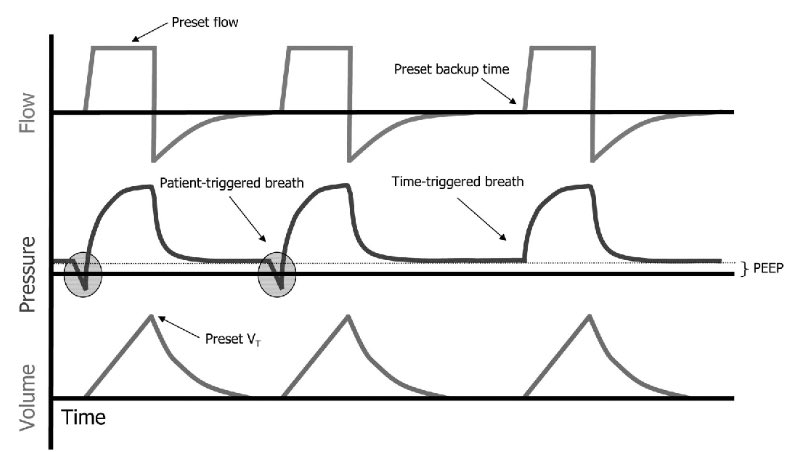
3/ Next, set the ventilator. You& #39;ll need to choose an initial setting.
Typically this will be assist control/volume control (AC/VC) which allows you to:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Maintain low tidal volume ventilation
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Maintain low tidal volume ventilation
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Guarantee a respiratory rate
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Guarantee a respiratory rate
Pic from https://bit.ly/3462mny ">https://bit.ly/3462mny&q...
Typically this will be assist control/volume control (AC/VC) which allows you to:
Pic from https://bit.ly/3462mny ">https://bit.ly/3462mny&q...
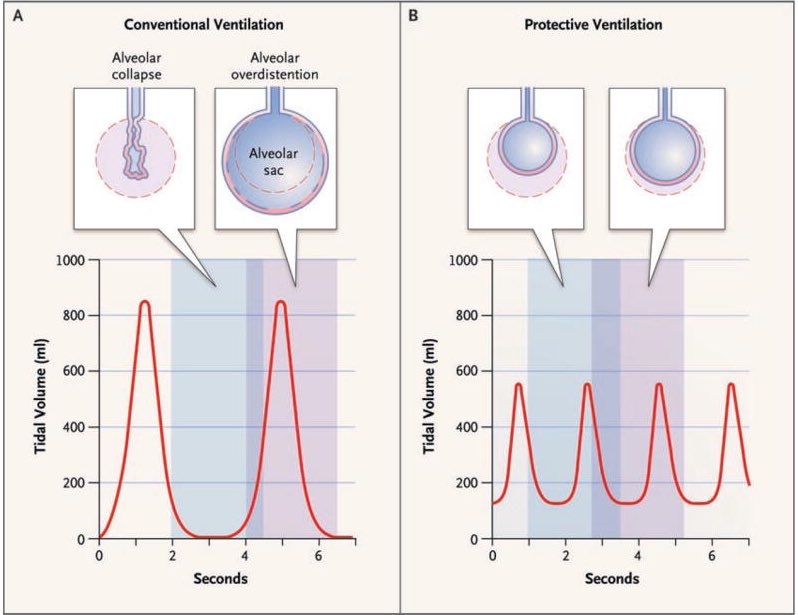
4/ You& #39;ll need to set minute ventilation (MV = tidal volume x respiratory rate)
-Try to approximate pre-intubation MV (not always possible)
-Use low tidal volume ventilation (4-8 ml/kg ideal body weight)
-Goal plateau pressure < 30 mmHg
-Goal pH > 7.2
https://www.ncbi.nlm.nih.gov/pubmed/17855672 ">https://www.ncbi.nlm.nih.gov/pubmed/17...
-Try to approximate pre-intubation MV (not always possible)
-Use low tidal volume ventilation (4-8 ml/kg ideal body weight)
-Goal plateau pressure < 30 mmHg
-Goal pH > 7.2
https://www.ncbi.nlm.nih.gov/pubmed/17855672 ">https://www.ncbi.nlm.nih.gov/pubmed/17...
5/ Finally, set PEEP/FiO2:
- Avoid O2 sats of 100% (hyperoxia is bad), aim for 92%-95%
- Set adequate PEEP, typically >10 mmHg in ARDS
COVID19 patients are PEEP-sensitive. In general aim for higher PEEP and lower FiO2. https://www.ebmedicine.net/topics/infectious-disease/COVID-19">https://www.ebmedicine.net/topics/in...
- Avoid O2 sats of 100% (hyperoxia is bad), aim for 92%-95%
- Set adequate PEEP, typically >10 mmHg in ARDS
COVID19 patients are PEEP-sensitive. In general aim for higher PEEP and lower FiO2. https://www.ebmedicine.net/topics/infectious-disease/COVID-19">https://www.ebmedicine.net/topics/in...
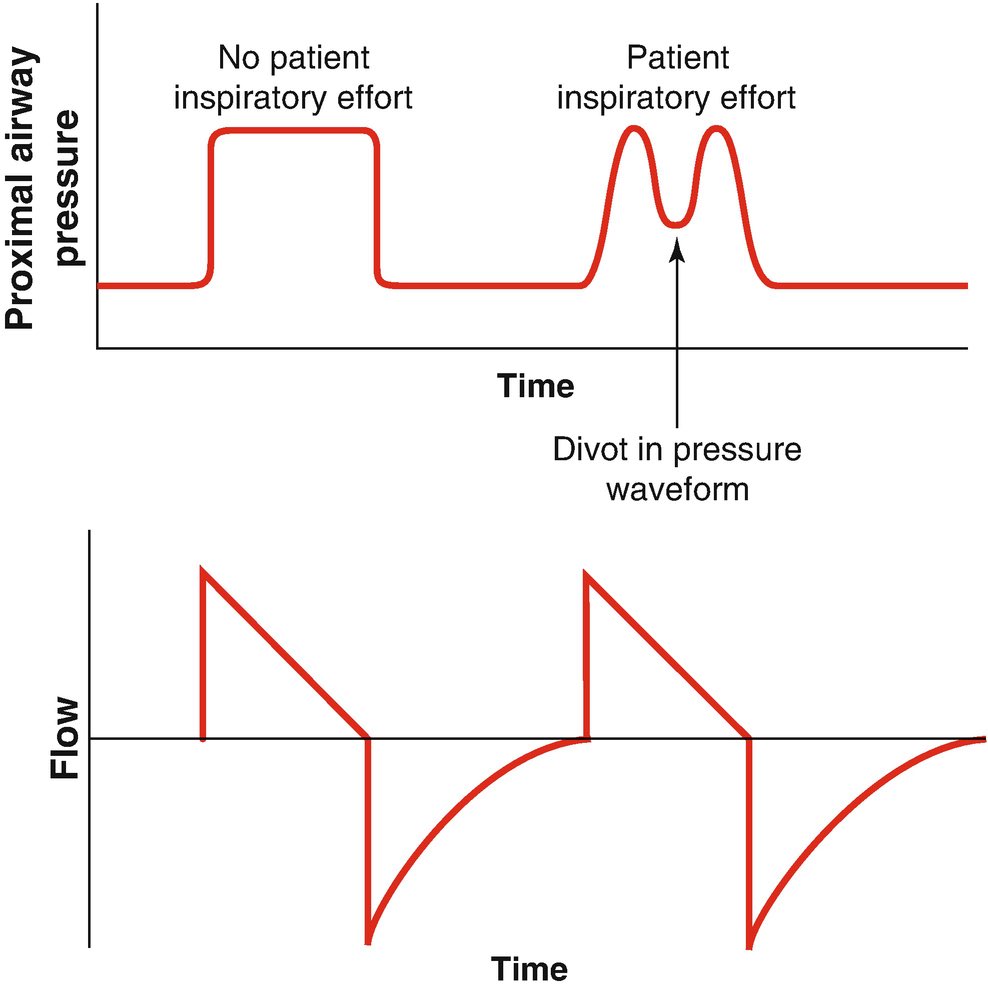
6/ Now that the ventilator& #39;s set, choose a sedation strategy.
- Patients with moderate to severe ARDS usually need sedation to ensure vent synchrony
- Vent Dyssynchrony https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> oxygenation and
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> oxygenation and  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> lung injury
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> lung injury
- Whatever sedation you choose, achieve synchrony
https://link.springer.com/chapter/10.1007/978-3-319-89981-7_7">https://link.springer.com/chapter/1...
- Patients with moderate to severe ARDS usually need sedation to ensure vent synchrony
- Vent Dyssynchrony
- Whatever sedation you choose, achieve synchrony
https://link.springer.com/chapter/10.1007/978-3-319-89981-7_7">https://link.springer.com/chapter/1...
7/ Some patients will oxygenate well with adequate PEEP and sedation.
Others will require additional therapies. Let& #39;s briefly review:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="😑" title="Expressionless face" aria-label="Emoji: Expressionless face">Paralysis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😑" title="Expressionless face" aria-label="Emoji: Expressionless face">Paralysis
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙃" title="Upside-down face" aria-label="Emoji: Upside-down face">Proning
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🙃" title="Upside-down face" aria-label="Emoji: Upside-down face">Proning
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="😮" title="Face with open mouth" aria-label="Emoji: Face with open mouth">Inhaled pulmonary vasodilators
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😮" title="Face with open mouth" aria-label="Emoji: Face with open mouth">Inhaled pulmonary vasodilators
Others will require additional therapies. Let& #39;s briefly review:
8/Who may require paralysis?
Those patients that remain dyssynchronous/hypoxemic despite sedation.
Paralysis does not improve mortality in severe ARDS but individual patients may benefit. https://www.nejm.org/doi/full/10.1056/NEJMoa1901686">https://www.nejm.org/doi/full/...
Those patients that remain dyssynchronous/hypoxemic despite sedation.
Paralysis does not improve mortality in severe ARDS but individual patients may benefit. https://www.nejm.org/doi/full/10.1056/NEJMoa1901686">https://www.nejm.org/doi/full/...
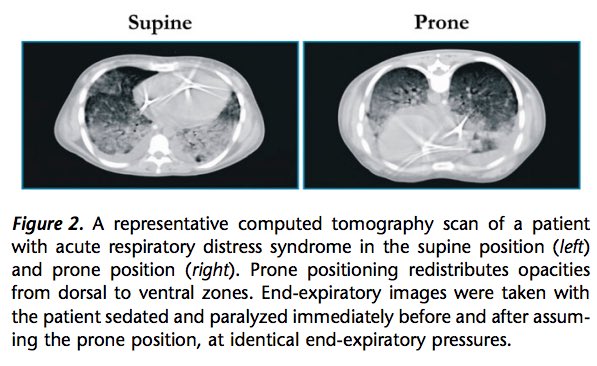
9/ Benefits of proning?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Turning patients to the prone position optimizes V/Q matching and lung recruitment, and may dramatically improve hypoxemia.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Turning patients to the prone position optimizes V/Q matching and lung recruitment, and may dramatically improve hypoxemia.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">It has been shown to reduce mortality in those with PaO2:FiO2 < 150.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">It has been shown to reduce mortality in those with PaO2:FiO2 < 150.
https://www.ncbi.nlm.nih.gov/pubmed/24134414 ">https://www.ncbi.nlm.nih.gov/pubmed/24...
https://www.ncbi.nlm.nih.gov/pubmed/24134414 ">https://www.ncbi.nlm.nih.gov/pubmed/24...
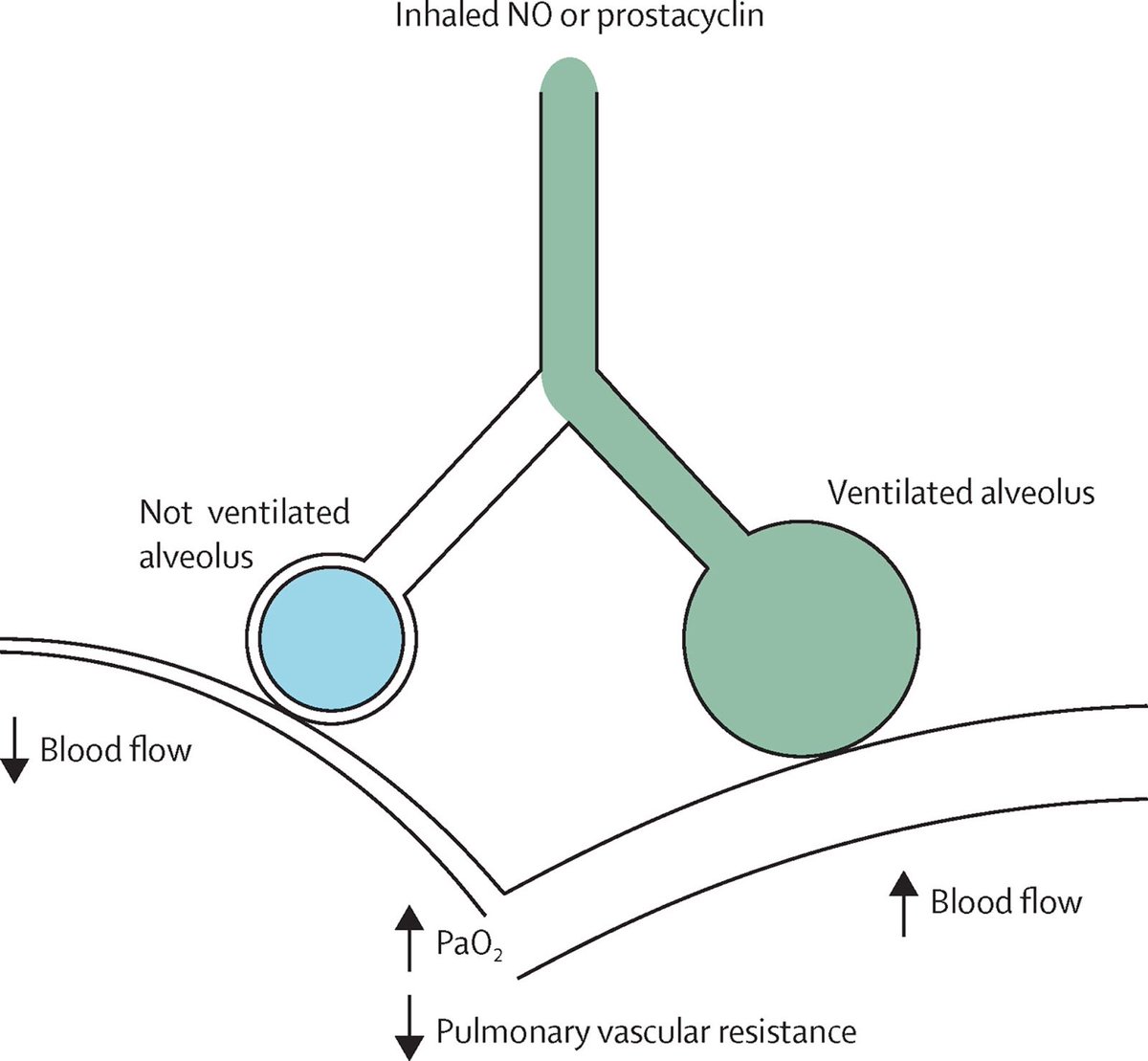
10/ What are ex. of inhaled pulmonary vasodilators?
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Epoprostenol or
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Epoprostenol or
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">nitric oxide
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">nitric oxide
- Preferentially vasodilate aerated lung units, https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> V/Q matching and
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> V/Q matching and  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SpO2
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SpO2
- No impact on mortality or lung mechanics so should only be added for refractory hypoxemia
https://www.ncbi.nlm.nih.gov/pubmed/27203510 ">https://www.ncbi.nlm.nih.gov/pubmed/27...
- Preferentially vasodilate aerated lung units,
- No impact on mortality or lung mechanics so should only be added for refractory hypoxemia
https://www.ncbi.nlm.nih.gov/pubmed/27203510 ">https://www.ncbi.nlm.nih.gov/pubmed/27...
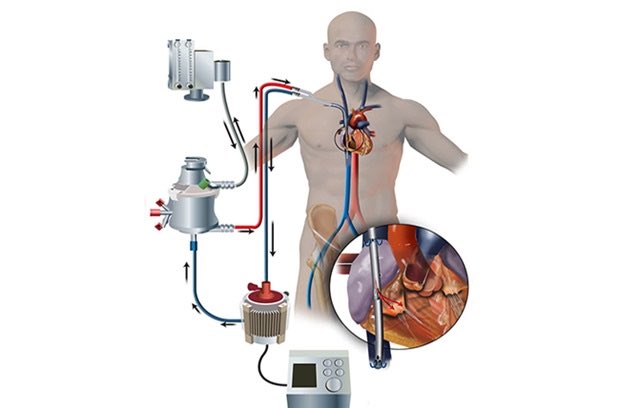
11/ Finally, when to call the veno-venous ECMO team.
There& #39;s no hard/fast rule but this is reserved for patients w/ refractory severe hypoxemia or respiratory acidosis despite conventional therapies.
A general rule is "it& #39;s better to call for ECMO too early than too late."
There& #39;s no hard/fast rule but this is reserved for patients w/ refractory severe hypoxemia or respiratory acidosis despite conventional therapies.
A general rule is "it& #39;s better to call for ECMO too early than too late."
12/ To summarize:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Confirm tube position
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Confirm tube position
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Low tidal volumes, adequate PEEP
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Low tidal volumes, adequate PEEP
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Tolerate respiratory acidosis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Tolerate respiratory acidosis
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Sedate for synchrony
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Sedate for synchrony
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> If still hypoxemic, prone and probably paralyze, inhaled vasodilators if refractory
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> If still hypoxemic, prone and probably paralyze, inhaled vasodilators if refractory
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Better to call for ECMO too early than too late
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Better to call for ECMO too early than too late

 Read on Twitter
Read on Twitter
 Maintain low tidal volume ventilationhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Guarantee a respiratory ratePic from https://bit.ly/3462mny&q..." title="3/ Next, set the ventilator. You& #39;ll need to choose an initial setting.Typically this will be assist control/volume control (AC/VC) which allows you to:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Maintain low tidal volume ventilationhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Guarantee a respiratory ratePic from https://bit.ly/3462mny&q..." class="img-responsive" style="max-width:100%;"/>
Maintain low tidal volume ventilationhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Guarantee a respiratory ratePic from https://bit.ly/3462mny&q..." title="3/ Next, set the ventilator. You& #39;ll need to choose an initial setting.Typically this will be assist control/volume control (AC/VC) which allows you to:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Maintain low tidal volume ventilationhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Guarantee a respiratory ratePic from https://bit.ly/3462mny&q..." class="img-responsive" style="max-width:100%;"/>
 oxygenation and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> lung injury- Whatever sedation you choose, achieve synchrony https://link.springer.com/chapter/1..." title="6/ Now that the ventilator& #39;s set, choose a sedation strategy.- Patients with moderate to severe ARDS usually need sedation to ensure vent synchrony- Vent Dyssynchrony https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> oxygenation and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> lung injury- Whatever sedation you choose, achieve synchrony https://link.springer.com/chapter/1..." class="img-responsive" style="max-width:100%;"/>
oxygenation and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> lung injury- Whatever sedation you choose, achieve synchrony https://link.springer.com/chapter/1..." title="6/ Now that the ventilator& #39;s set, choose a sedation strategy.- Patients with moderate to severe ARDS usually need sedation to ensure vent synchrony- Vent Dyssynchrony https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Downwards arrow" aria-label="Emoji: Downwards arrow"> oxygenation and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> lung injury- Whatever sedation you choose, achieve synchrony https://link.springer.com/chapter/1..." class="img-responsive" style="max-width:100%;"/>
 Turning patients to the prone position optimizes V/Q matching and lung recruitment, and may dramatically improve hypoxemia.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">It has been shown to reduce mortality in those with PaO2:FiO2 < 150. https://www.ncbi.nlm.nih.gov/pubmed/24..." title="9/ Benefits of proning?https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Turning patients to the prone position optimizes V/Q matching and lung recruitment, and may dramatically improve hypoxemia.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">It has been shown to reduce mortality in those with PaO2:FiO2 < 150. https://www.ncbi.nlm.nih.gov/pubmed/24..." class="img-responsive" style="max-width:100%;"/>
Turning patients to the prone position optimizes V/Q matching and lung recruitment, and may dramatically improve hypoxemia.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">It has been shown to reduce mortality in those with PaO2:FiO2 < 150. https://www.ncbi.nlm.nih.gov/pubmed/24..." title="9/ Benefits of proning?https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">Turning patients to the prone position optimizes V/Q matching and lung recruitment, and may dramatically improve hypoxemia.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark">It has been shown to reduce mortality in those with PaO2:FiO2 < 150. https://www.ncbi.nlm.nih.gov/pubmed/24..." class="img-responsive" style="max-width:100%;"/>
 Epoprostenol or https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">nitric oxide- Preferentially vasodilate aerated lung units, https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> V/Q matching and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SpO2- No impact on mortality or lung mechanics so should only be added for refractory hypoxemia https://www.ncbi.nlm.nih.gov/pubmed/27..." title="10/ What are ex. of inhaled pulmonary vasodilators?https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Epoprostenol or https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">nitric oxide- Preferentially vasodilate aerated lung units, https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> V/Q matching and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SpO2- No impact on mortality or lung mechanics so should only be added for refractory hypoxemia https://www.ncbi.nlm.nih.gov/pubmed/27..." class="img-responsive" style="max-width:100%;"/>
Epoprostenol or https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">nitric oxide- Preferentially vasodilate aerated lung units, https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> V/Q matching and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SpO2- No impact on mortality or lung mechanics so should only be added for refractory hypoxemia https://www.ncbi.nlm.nih.gov/pubmed/27..." title="10/ What are ex. of inhaled pulmonary vasodilators?https://abs.twimg.com/emoji/v2/... draggable="false" alt="1️⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one">Epoprostenol or https://abs.twimg.com/emoji/v2/... draggable="false" alt="2️⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two">nitric oxide- Preferentially vasodilate aerated lung units, https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> V/Q matching and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Upwards arrow" aria-label="Emoji: Upwards arrow"> SpO2- No impact on mortality or lung mechanics so should only be added for refractory hypoxemia https://www.ncbi.nlm.nih.gov/pubmed/27..." class="img-responsive" style="max-width:100%;"/>