Starting a series on clinical Pearls I am gathering in #COVID19 patients based on experiences of many experts
Will add as we go along
Feel free to add your own observations/experiences
#covidclinicalpearls /1
Will add as we go along
Feel free to add your own observations/experiences
#covidclinicalpearls /1
Anosmia is likely the most specific #COVID19 related symptom
30% of patients have anosmia as their 1st symptom
#covidclinicalpearls /2
30% of patients have anosmia as their 1st symptom
#covidclinicalpearls /2
Around 90% of patients have fever.
50% maybe afebrile at the time of presentation
Fever tends to be very resistant to routine measures in hospitalized patients
There is no consensus that NSAIDs are to be avoided in #COVID2019 patients
#covidclinicalpearls /3
50% maybe afebrile at the time of presentation
Fever tends to be very resistant to routine measures in hospitalized patients
There is no consensus that NSAIDs are to be avoided in #COVID2019 patients
#covidclinicalpearls /3
Viral shedding is greatest at the time of symptom onset and declines over the course of several days
50% of patients keep shedding after complete resolution of symptoms
Viral shedding can continue for as much as 24 days
#COVID2019
#covidclinicalpearls /4
50% of patients keep shedding after complete resolution of symptoms
Viral shedding can continue for as much as 24 days
#COVID2019
#covidclinicalpearls /4
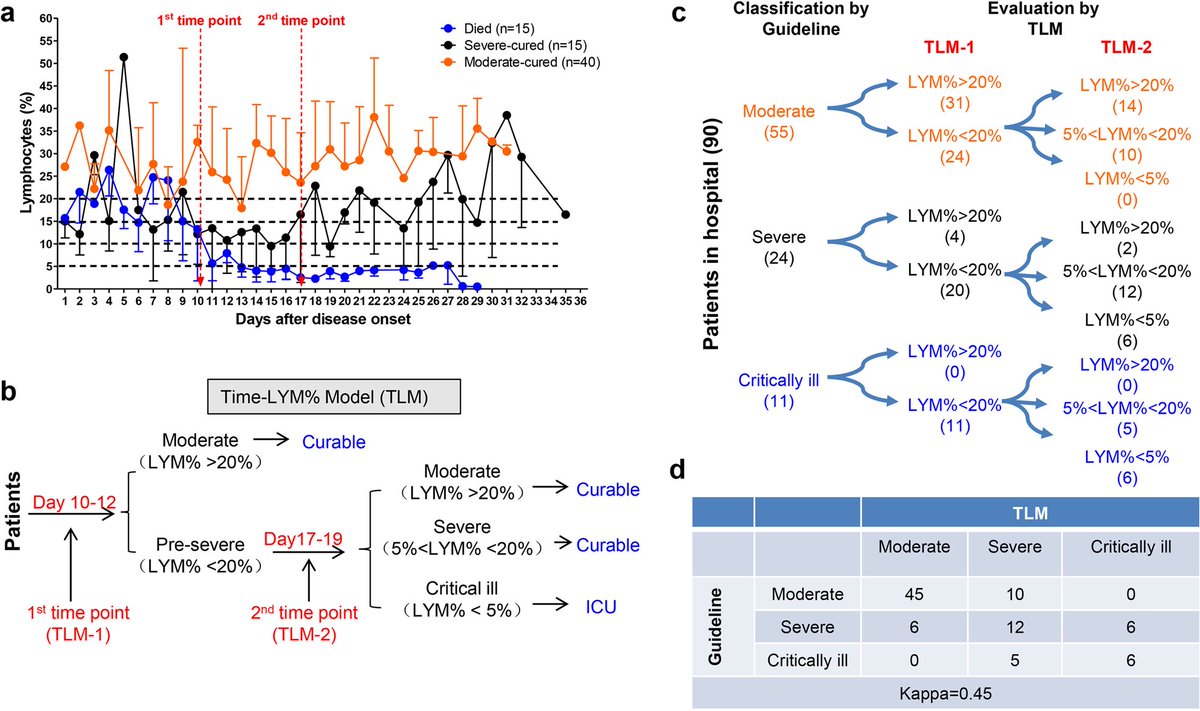
Lymphopenia is common in #COVID2019 > 80% patients
Leukopenia is seen in 1/3 of patients
Its associates with poor outcomes and poor surivival.
Recovery with Lym % > 20% at Day10 of symptoms is a + outcome marker
Lym % of <5% = poor prognosis
#covidclinicalpearls /5
Leukopenia is seen in 1/3 of patients
Its associates with poor outcomes and poor surivival.
Recovery with Lym % > 20% at Day10 of symptoms is a + outcome marker
Lym % of <5% = poor prognosis
#covidclinicalpearls /5
Lymphopenia timeline in #COVID19
LYM% < 20% are pre-severe type
At TLM-2
If LYM% > 20% those are reclassified as “moderate”
If 5% < 20% = “severe”
If < 5% = “critical”
#covidclinicalpearls /6
LYM% < 20% are pre-severe type
At TLM-2
If LYM% > 20% those are reclassified as “moderate”
If 5% < 20% = “severe”
If < 5% = “critical”
#covidclinicalpearls /6
Diagnosis by PCR testing has upto 30% false negative rate #COVID19
Sampling early in disease course will have lower sensitivity
CT Chest has BETTER predictive value in cases where CT findings are high probability even if PCR swab negative
#covidclinicalpearls /7
Sampling early in disease course will have lower sensitivity
CT Chest has BETTER predictive value in cases where CT findings are high probability even if PCR swab negative
#covidclinicalpearls /7
Average time from initial negative to positive PCR swab test is 5 days
Do NOT rule out #COVID19 with ONE pharyngeal swab.
Sensitivity of CT in patients with positive CT & negative PCR is 97%
#covidclinicalpearls /8
Do NOT rule out #COVID19 with ONE pharyngeal swab.
Sensitivity of CT in patients with positive CT & negative PCR is 97%
#covidclinicalpearls /8
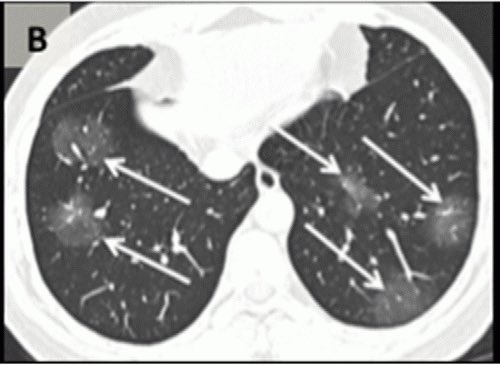
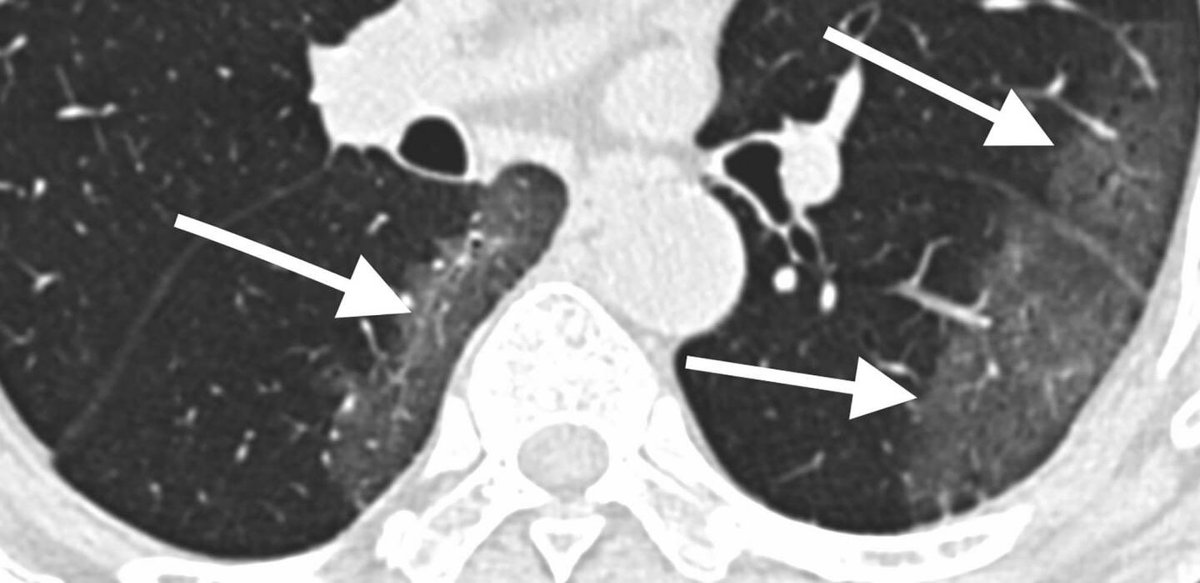
#CT Chest in #COVID19
Early #groundglass abnormality in early disease,
followed by “crazy paving,”
finally increasing consolidation
Typically peripheral
#covidclinicalpearls /9
Early #groundglass abnormality in early disease,
followed by “crazy paving,”
finally increasing consolidation
Typically peripheral
#covidclinicalpearls /9
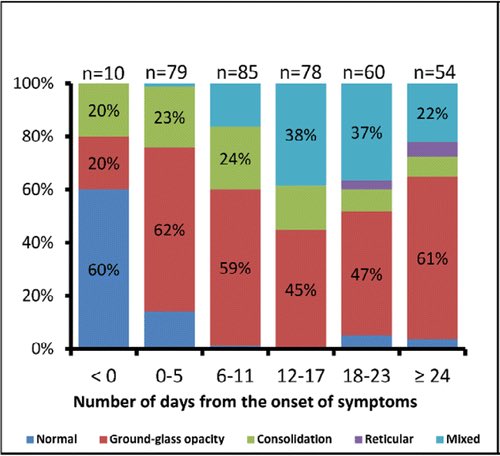
Temporal changes of CT findings in #COVID19
Note #groundglass predominant early
#covidclinicalpearls /10
Note #groundglass predominant early
#covidclinicalpearls /10
Respiratory support
#COVID19
AVOID
- Noninvasive ventilations #NPPV
- High flow O2 #HFNC
due to high risk to healthcare workers due to aerosols.
EARLY intubation
#covidclinicalpearls /11
#COVID19
AVOID
- Noninvasive ventilations #NPPV
- High flow O2 #HFNC
due to high risk to healthcare workers due to aerosols.
EARLY intubation
#covidclinicalpearls /11
For #intubation in #COVID19
Only Experts intubate
AVOID bag-mask ventilations
Use PEEP valve if needed
Gentle bagging via supraglottic device preferred if needed
Always use rapid sequence intubation - rocuronium preferred by some
#covidclinicalpearls /12
Only Experts intubate
AVOID bag-mask ventilations
Use PEEP valve if needed
Gentle bagging via supraglottic device preferred if needed
Always use rapid sequence intubation - rocuronium preferred by some
#covidclinicalpearls /12
If using #NPPV #NIV in #COVID2019 ( #Ventilator in short supply)
Use a full face mask or helmet
Use a filter for the leak port
Use a HME Filter to provide additional safety from aerosol
Set Alarms for patient disconnect
#covidclinicalpearls /13
Use a full face mask or helmet
Use a filter for the leak port
Use a HME Filter to provide additional safety from aerosol
Set Alarms for patient disconnect
#covidclinicalpearls /13
If using #HFNC (preferred to #NIV) in #COVID19
Use preferably low flow rates (30-40L/min) have lower rates of aerosolization
Always increase FiO2 to max before increasing flow rate >30L/min
Reassess at 1 hr and 3 hr intervals for possible intubation
#covidclinicalpearls /14
Use preferably low flow rates (30-40L/min) have lower rates of aerosolization
Always increase FiO2 to max before increasing flow rate >30L/min
Reassess at 1 hr and 3 hr intervals for possible intubation
#covidclinicalpearls /14
Use of Venturi mask
#COVID19
if patient requires >8L/min NC
Non humidified
Uptitrate to FiO2 35%
Then increase flow rate if needed to 12 L/min
#covidclinicalpearls /15
#COVID19
if patient requires >8L/min NC
Non humidified
Uptitrate to FiO2 35%
Then increase flow rate if needed to 12 L/min
#covidclinicalpearls /15
For mechanical #ventilation in #COVID19 #ICU
Tidal volume 6ml/kg IBW
PEEP 5 if BMI <35
(10 if BMI >35)
Avoid HIGH PEEP
#COVID19 ARDS is atypical with normal compliance & high PEEP may do more harm than good
#covidclinicalpearls /16
Tidal volume 6ml/kg IBW
PEEP 5 if BMI <35
(10 if BMI >35)
Avoid HIGH PEEP
#COVID19 ARDS is atypical with normal compliance & high PEEP may do more harm than good
#covidclinicalpearls /16
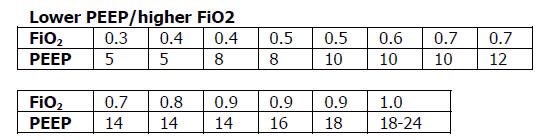
Use ARDSnet LOW PEEP table as a guide but try to maintain as low a PEEP as feasible early in #COVID19 disease
#covidclinicalpearls /17
#covidclinicalpearls /17

 Read on Twitter
Read on Twitter