Creating my first tweet thread on transferring #COVID19 ED pts to the ICU and running IV pumps from the hall from a pharmacist perspective. This is very basic but I hope it& #39;s helpful.
When the ED calls to give report on patient transferring to the unit, assuming they are running on multiple drips - get your unit& #39;s pumps and poles ready. The ED is definitely short on these so you& #39;re giving theirs back.
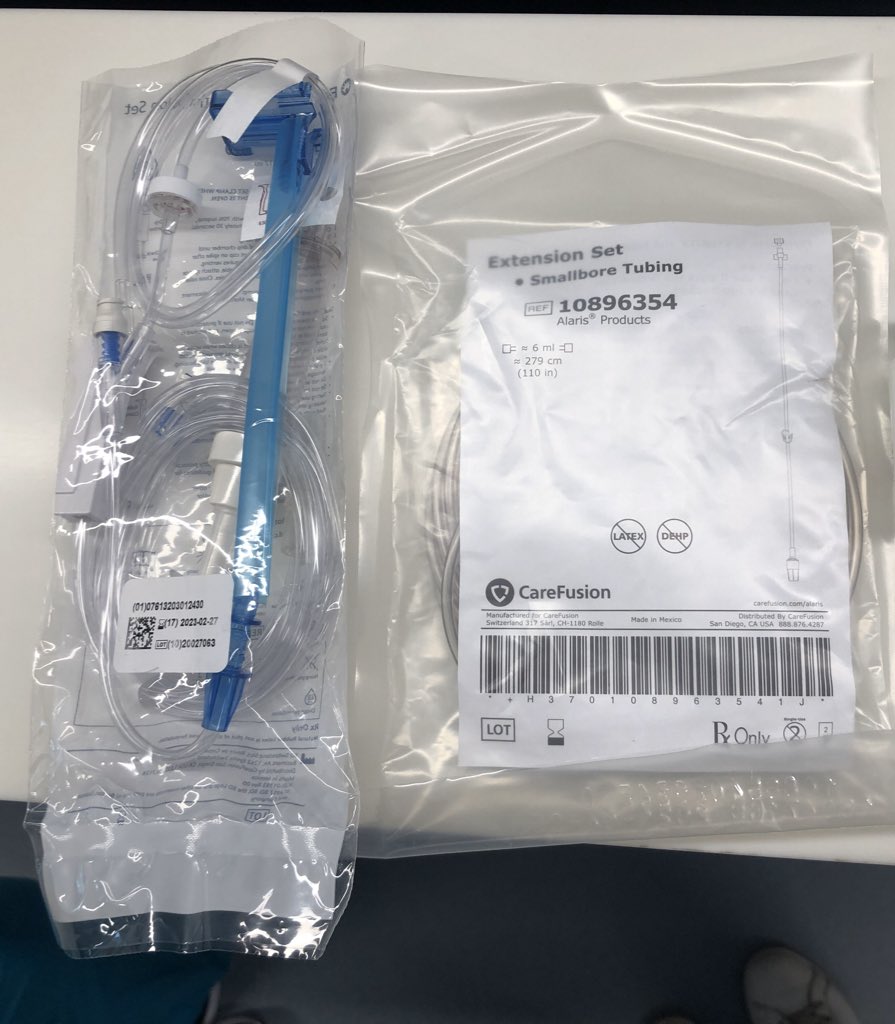
Grab regular IV tubing if you& #39;re spiking new bags and 1-2 sets of extension tubing per each drip. If their bags are full, have some sort of wipes available to clean any IV bags and lines that have been in their room.
Send the nurse in the room with the extension tubing. Throw a baby monitor in the room if you have one so the nurses can tell you what they need without any extra opening of the doors. Let the nurses get the pt settled. If you& #39;re on the unit, your extra set of hands is invaluable
Pharmacists - wear an N95 and gloves at minimum because there will be unavoidable door opening. After the pt is settled in and the nurses are ready, it& #39;s time to transfer the meds. Inside the room they will hook up the extension tubing to the pt and regular IV tubing.
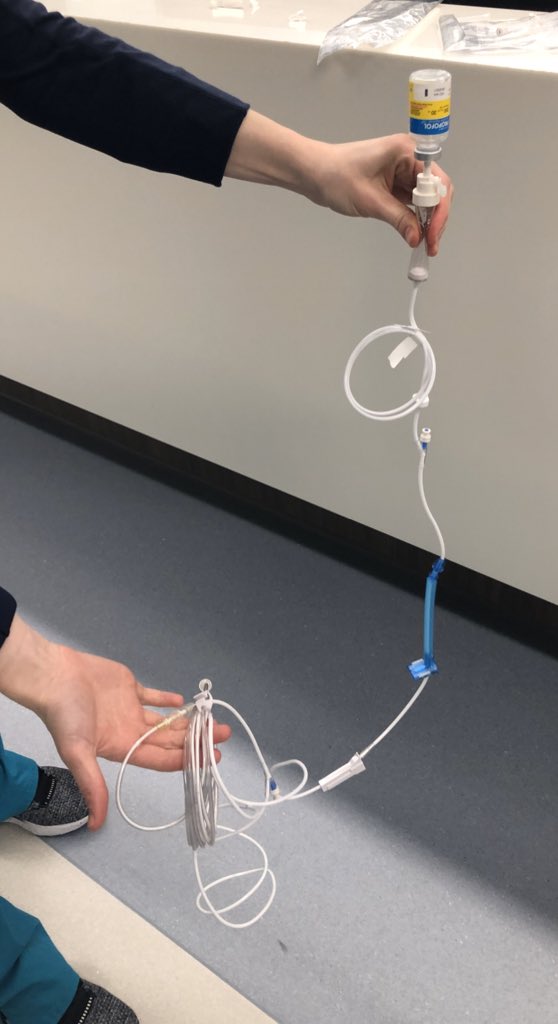
Depending on the size of the room and line placement, you may need to relocate the bed. We are moving the beds ~2-3 feet closer to the door. Inside the room, each bag can get wiped down before getting handed out - then give the bags/lines a second cleaning outside the room.
If you didn& #39;t hear what rates your meds are running at, this is where the baby monitor becomes  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Key" aria-label="Emoji: Key">. As they transfer the meds out you can communicate through the monitors to set up the new pump at the same rates.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🔑" title="Key" aria-label="Emoji: Key">. As they transfer the meds out you can communicate through the monitors to set up the new pump at the same rates.
3M hooks inside the room on the back of the door have been helpful for grouping lines together to reduce any tripping hazards. If you have a lot of slack outside the room, we have used the latex tourniquets to create a loop and bundle the lines to hang from the pole.
We have windows on our doors. Before trialing this on a COVID pt, we made sure we could scan bags through windows. It does work but you may need a pal to get the barcode pretty close to the glass.
If you don& #39;t have a baby monitor, laminated sheets of paper become a whiteboard to help communicate. Our doors are thick and yelling through them in an N95 is not fun
Use some sort of stickers to add a date and time to the lines.
If you need to run antibiotics, try and run them secondary on a TKO fluid. Push whatever is pushable. Otherwise you& #39;ll lose most of the first dose in the extension tubing. Our nurses aren& #39;t restringing every single dose.
We - aka @gmjones09 - found the 20mL propofol priming how-to on Twitter. Made a step by step guide and it& #39;s going great - uses up our stock of small vials to conserve our large ones.
After your set up is complete - give those analgesics and sedatives a clinical look. Try and wean down anything that may have been cranked up during the initial frenzy. Conservation is key during these shortages. We are touching base at least 2x a day to see how we can cut down.
Start this process one bed at a time. If you have non-COVID patients, try it on one or two ahead of time to work out the kinks because it more difficult for pts on isolation. Train a few nurses to become experts. They can train more nurses and hand it off to the next shift.
Your ICU is going to be busy and you& #39;re definitely going to see new nursing faces each day. Introduce yourself to all that are new to your unit so they know who to grab when they have questions. As we started cohorting, there& #39;s been a mix of ICU, step down, and med-surg nurses
Please add any other advice/tips you might have!

 Read on Twitter
Read on Twitter