A thread about ICU admission decisions
There seems to be lots of (mis)information about how intensive care doctors decide whether a patient would benefit from coming to ICU. I thought I’d try and explain some of these decisions - relevant to Covid and more generally.
1/n
There seems to be lots of (mis)information about how intensive care doctors decide whether a patient would benefit from coming to ICU. I thought I’d try and explain some of these decisions - relevant to Covid and more generally.
1/n
ICU isn’t a magic treatment. We offer organ support, e.g. ventilation, or blood pressure support, to help the sickest patients recover from their illness. It offers high levels of nursing & medical input and close monitoring.
2/n
2/n
It is not a treatment in itself and the patient has to be able to get better - ICU supports them do this.
There a key considerations intensivists will make when considering if someone should be admitted to ICU...
3/n
There a key considerations intensivists will make when considering if someone should be admitted to ICU...
3/n
The current illness:
What is the patient ill with? If it is a pneumonia, how serious is it? How much oxygen are they requiring? Is their breathing laboured? If their pneumonia is very bad and they maybe need ventilation, is this going to help the patient get better?
4/n
What is the patient ill with? If it is a pneumonia, how serious is it? How much oxygen are they requiring? Is their breathing laboured? If their pneumonia is very bad and they maybe need ventilation, is this going to help the patient get better?
4/n
Covid is a good example where, for some patients, they do not need to come to ICU as they may be fine on facemask oxygen or NIV facemask on the wards. Some may need to come in a few days perhaps.
5/n
5/n
Their longterm illnesses and physical state
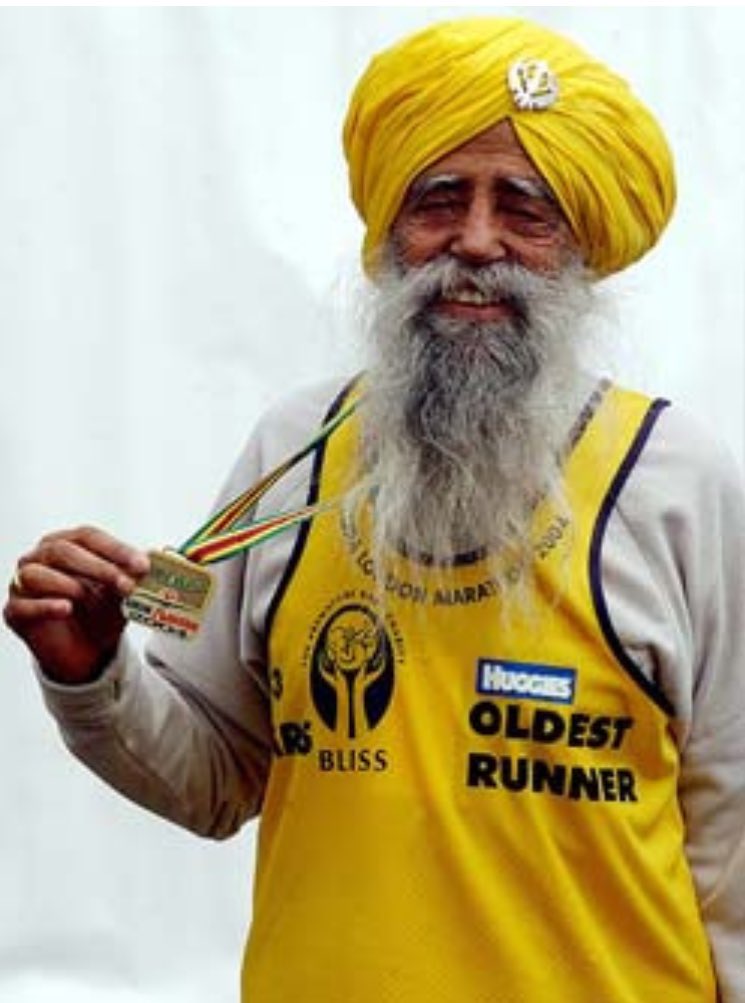
What can this person do normally? Are they able to run a marathon? Or are they bed bound? Are they are physically fit normally or conversely frail? If so, they are much more likely to be able to fight the disease and recover.
6/n
What can this person do normally? Are they able to run a marathon? Or are they bed bound? Are they are physically fit normally or conversely frail? If so, they are much more likely to be able to fight the disease and recover.
6/n
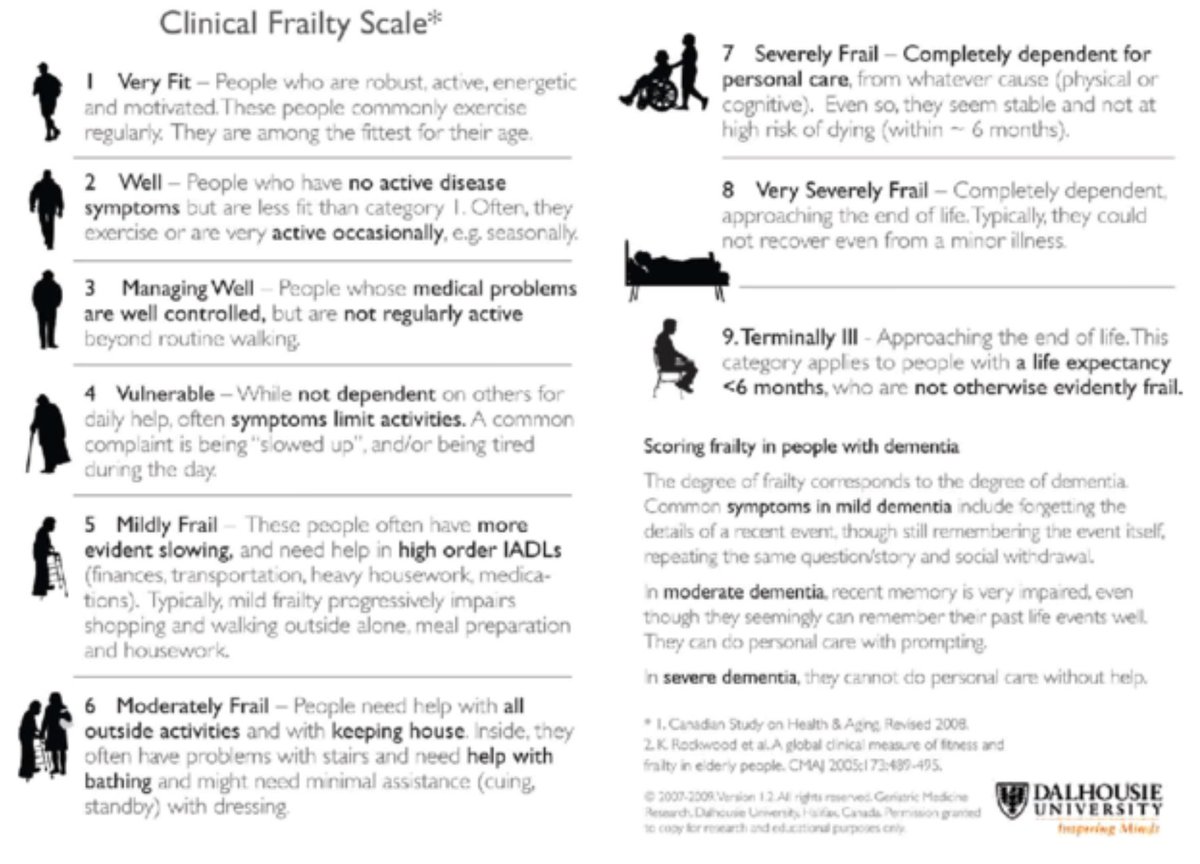
If they are very weak, frail and deconditioned, they are less likely to have the ability to fight the disease. This is what we call physiological reserve - how good is their body going to be at fighting this disease?
7/n
7/n
Actual age is irrelevant. It is physiological age that matters. If they are an 70 year old with no medical problems and active they have a much better ‘physiological reserve’ than someone in their 50s who has had multiple heart attacks, ...
8/n
8/n
been in and out of hospital with difficult diabetes, has bad kidney function and can’t manage to walk more than 50m before getting short of breath.
Our machines and drugs can support the body, but ultimately the patient has to be able to support themselves.
9/n
Our machines and drugs can support the body, but ultimately the patient has to be able to support themselves.
9/n
Recoverability
If the acute illness is so bad, then whatever we do, ICU will not change the outcome. The illness maybe recoverable in a fit person, but perhaps the patient has so many other medical problems their body won’t be able to cope with the illness ontop.
10/n
If the acute illness is so bad, then whatever we do, ICU will not change the outcome. The illness maybe recoverable in a fit person, but perhaps the patient has so many other medical problems their body won’t be able to cope with the illness ontop.
10/n
Recovery beyond ICU is essential. Leaving ICU is just the start of a journey with critical illness. Many people take months-years to recover from an ICU illness.
11/n
11/n
Serious illness leads to loss of muscle tissues, weakened immune systems, worse brain function (confusion, memory loss, PTSD), poor cough, shortness of breath, to name a few problems. People have be able to be strong enough for rehab and get through this recovery phase.
12/n
12/n
Patient’s wishes:
We alway ask patients how they would like to be treated. We won’t offer treatments we think are futile - will have no difference to their outcomes.
13/n
We alway ask patients how they would like to be treated. We won’t offer treatments we think are futile - will have no difference to their outcomes.
13/n
If patients are too unwell to tell us, then we ask family. This is not to ask what the family would want to happen to their relative. It is to gauge whether their ill relative had previously said what they would like to happen to them if they were be become very unwell.
14/n
14/n
Do they hate being ill and going to doctors? “They’d never want to end up on a ventilator and stuck in a chair all day” is a common thing relatives tell us. The last thing we want to do is put someone through an ICU admission if they never want it.
15/n
15/n
Perhaps, worse would be if they got through their admission, but then died on the wards later on because they were too weak to recover from their illness. The traumatic experiences & struggles of getting through an ICU stay need to be worth it - for the pt, their family
16/n
16/n
These are complex & difficult decisions. Different Intensivists may make different decisions. There are no right answers. A collective approach of with intensivists, specialist docs with patients & their families, we hope we make the right decision for each patient.
17/n
17/n
In conclusion, when admitting someone to ICU, intensivists consider:
- The current illness
- The baseline function of patient including other illnesses
- The patient’s wishes
18/n
- The current illness
- The baseline function of patient including other illnesses
- The patient’s wishes
18/n

 Read on Twitter
Read on Twitter