THREAD PART II of II: To mask or not to mask?
Now to explore modern day implications regarding airborne spread...
1/15
Now to explore modern day implications regarding airborne spread...
1/15
First let’s officially define contact vs airborne.
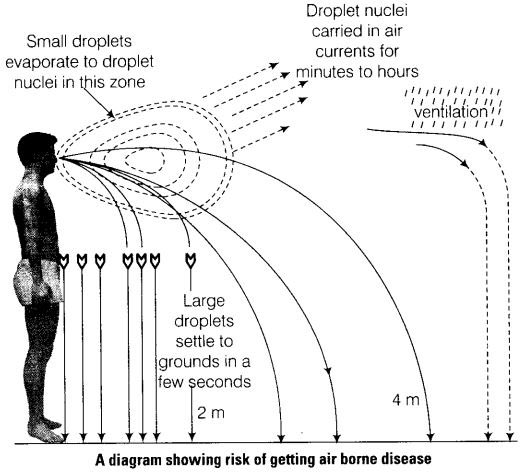
Contact spread includes large droplets (>5 microns, or which fall before they evaporate).
Airborne spread includes small droplets (<5 microns, or which evaporate before they fall).
2/
Contact spread includes large droplets (>5 microns, or which fall before they evaporate).
Airborne spread includes small droplets (<5 microns, or which evaporate before they fall).
2/
But as others have mentioned, this dichotomous definition includes neither the fluid dynamics of droplets, nor the continuum of droplet sizes.
3/
3/
Droplets that are spread via a sneeze, cough, or simple exhalation behave more like a cloud. Some of them will fall to the ground, some will rise towards the ceiling, some will linger in the air, and some will evaporate.
4/
4/
Thus we should not be surprised that Dr. Fineberg of the National Academies of Sciences, Engineering, and Medicine confirmed today that studies indicate SARS-CoV-2 can be aerosolized via normal breathing.
5/
5/
When we discuss “contact” vs “airborne”, what matters is whether the small droplets that linger in the air can cause disease. For SARS-CoV-2, it seems that - as the WHO has stated - MOST cases are not spread this way.
However, there are exceptions...enough to be cautious.
6/
However, there are exceptions...enough to be cautious.
6/
For comparison, we can look towards SARS-CoV outbreaks that occurred on flights in 2003. During one 3-hour flight from Hong Kong to Beijing with 120 people on board, 1 infected person caused SARS infections in 20 other people (2 crew members not depicted in this image).
7/
7/
In simulated cases of droplet spread in this case, >99% of the aerosols were deposited. However passenger movement had a strong influence, and could re-distribute some of the aerosols that had previously landed. This likely led to the atypical spread pattern.
8/
8/
One can imagine that in similar small, crowded spaces (such as a hospital room or OR), it would be quite easy to stir up aerosols or get caught in an aerosolized cloud. There are anecdotes of this.
In other situations, like an outdoor park, this would be less likely.
9/
In other situations, like an outdoor park, this would be less likely.
9/
Two such andecdotes below:
The now-infamous choir case: https://www.latimes.com/world-nation/story/2020-03-29/coronavirus-choir-outbreak
The">https://www.latimes.com/world-nat... case of a pituitary surgery in Wuhan gone wrong: https://www.entnet.org/sites/default/files/uploads/covid-19_endosb_lettertoeditor_neurosurgery_update3.23.20.pdf
10/">https://www.entnet.org/sites/def...
The now-infamous choir case: https://www.latimes.com/world-nation/story/2020-03-29/coronavirus-choir-outbreak
The">https://www.latimes.com/world-nat... case of a pituitary surgery in Wuhan gone wrong: https://www.entnet.org/sites/default/files/uploads/covid-19_endosb_lettertoeditor_neurosurgery_update3.23.20.pdf
10/">https://www.entnet.org/sites/def...
But hold up, this is not miasma. These are tiny particles from which we now have the ability to protect ourselves, right?
So what’s the deal with masks and when should we wear them?
11/
So what’s the deal with masks and when should we wear them?
11/
As we’ve seen, it can takes YEARS to conduct proper research about airborne risk...time we don’t have.
So if you are a healthcare worker, then you should absolutely wear a mask in a hospital ward with COVID-19 patients. Based on data available, an N95 would be safest.
12/
So if you are a healthcare worker, then you should absolutely wear a mask in a hospital ward with COVID-19 patients. Based on data available, an N95 would be safest.
12/
If you are a layperson hanging out at least 6 feet apart from others in a park, then you are likely safe from the 99% of droplets that cause disease. A mask may give you a sense of security, similar to a handkerchief dipped in aromatic oils.
(Please don’t hoard them though).
13/
(Please don’t hoard them though).
13/
History has demonstrated that it takes many, many years of research to determine whether a virus is airborne.
SARS-CoV-2 will be no different.
14/
SARS-CoV-2 will be no different.
14/
Thank you for listening to my Med Talk  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤗" title="Hugging face" aria-label="Emoji: Hugging face"> (and sorry it was so long!)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤗" title="Hugging face" aria-label="Emoji: Hugging face"> (and sorry it was so long!)
15/ END
15/ END

 Read on Twitter
Read on Twitter