"Cytokine Storm". The idiot& #39;s buzzword of the week. It makes you sound smarter if you say it often enough. When I first heard of it in 1994 it sounded AMAZING! Then this RCT came out showing it increased mortality. Ouch https://www.nejm.org/doi/full/10.1056/nejm199606273342603">https://www.nejm.org/doi/full/...
Next came rhAPC (drotrecogin). Don& #39;t knock out the immune system: we need it to survive. APC has signalling properties to modulate inflammation. NEJM PROWESS was touted a success! https://www.nejm.org/doi/full/10.1056/NEJM200103083441001">https://www.nejm.org/doi/full/...
Just as we were celebrating and retrospective analyses showed efficacy correlated with drotrecogin reducing Il-6 levels, bad news came in and the dream turned sour https://www.nejm.org/doi/full/10.1056/NEJMoa1202290">https://www.nejm.org/doi/full/...
These treatments looked so promising in animals models, in phase 1, 2 & 3 trials. All to no avail. For some, like me, the dream lives on! One day the right modulatory agent will be found. But IL-6 inhibitors are too crude a therapy https://jamanetwork.com/journals/jama/fullarticle/2763802">https://jamanetwork.com/journals/...
We are facing a crisis from a virus against which we have no proven treatments. Repeating the phrase "cytokine storm" as your infinite mantra as you resort to cavalier adventurism out of sheer panic violates the principle of DO NO HARM #CytokineStorm #COVID4MDs #FOAMcovid
I really do want to see progress with immuno(thrombo)modulation of sepsis/SIRS but it& #39;s seen so many setbacks. I can list many promising avenues for the future. But rash experimentation risks bringing it more into disrepute if it increases mortality. We don& #39;t want that #COVID4MDs
Another caveat. Historically, immuno(thrombo)modulation of a decompensated immune response = 2nd line therapy after failure to respond to appropriate antibiotic treatment. Immunosuppression without any effective antiviral treatment is a whole new ballgame #COVID4MDs
@Nature publishes misgivings similar to my own about the rush to treat COVID-19 with immunosuppressants. Using the term "cytokine STORM" as a call to action instead of "cytokine release syndrome" is another problem https://www.nature.com/articles/d41586-020-01056-7?utm_source=twitter&utm_medium=social&utm_content=organic&utm_campaign=NGMT_USG_JC01_GL_Nature">https://www.nature.com/articles/... #COVID4MDs
That Nature article failed to give sufficient warning about the potential dangers of steroids for #COVIF19. This Lancet article argues that steroids should only be given as part of an RCT https://twitter.com/TheLancet/status/1225429077735010304?s=20">https://twitter.com/TheLancet...
My next objection to a mad rush to immunosuppress after declaring the immune system public enemy number 1. There is lymphopoenia in COVID-19 as in HIV. Are we already too immunosuppressed? https://twitter.com/ToshiAkima/status/1251512431437729793?s=20">https://twitter.com/ToshiAkim...
Another objection to Il-6 blockers. We scream the "cytokine storm" mantra, meaning that an immune response is good but too much of a good thing is bad. Doesn& #39;t that mean we want to reduce excess Il-6 down to an ideal therapeutic range? Who checks Il-6 levels before and after Rx?
The truth is that nobody has done a large animal COVID-19 dose titration study to find what the optimal Il-6 level is in sepsis, let alone a Phase I clinical trial in humans. You just assume Il-6 = BAD. Ergo knock it out completely, the lower the Il-6 level the better. Why?
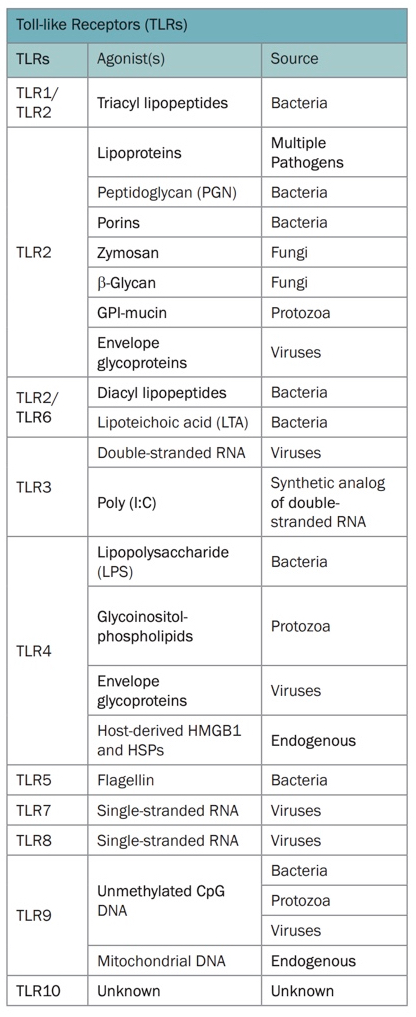
Next possible issue with Il-6 inhibitors. More men die from COVID-19 than women. TLR7 is inherited on the X chromosome. Women transcribe from both copies of the gene resulting in macrophages, NK cells, dendritic cells, lymphocytes expressing more TLR7 https://immunology.sciencemag.org/content/3/19/eaap8855">https://immunology.sciencemag.org/content/3...
TLR7 allows the innate immune system to recognise single-stranded RNA viruses like SARS-COV-2. If women express twice as much TLR7 than men this may result in more efficient viral clearance, improving outcomes https://www.cell.com/pb-assets/products/nucleus/nucleus-phagocytes/rnd-systems-tlr-br.pdf">https://www.cell.com/pb-assets...
But TLR7 also drives the output of Il-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2951126/">https://www.ncbi.nlm.nih.gov/pmc/artic... The reason for the lower mortality from COVID-6 in women might be due to a brisker TLR7 mediated Il-6 immune response. Il-6 might be the fire engine rather than the fire storm.

 Read on Twitter
Read on Twitter