Time for ventilator basics for the non-ICU nurse ! This is a super basic quick reference , there are plenty more ways to learn about vents , this is the down and dirt . Also AACN has made COVID learning modules free for anyone who wants more education !
Endotracheal tube(ETT): the actual tube that’s goes down into a pt’s lungs. It has a ballon on the end that is inflated to keep it in place, but should ALWAYS be secured with an ETT holder. Document the location of the ETT (ex:24cm at the lower lip) after placement is confirmed
& check at the beginning , end, & throughout your shift for movement or dislodgment. Respiratory Therapist should be checking the balloon inflation (or cuff pressure) q4. If you hear gurgling (& it’s not from oral secretions) ,
especially if paired with low alarm, it could be air leaking around the balloon, call RT and ask them to check.
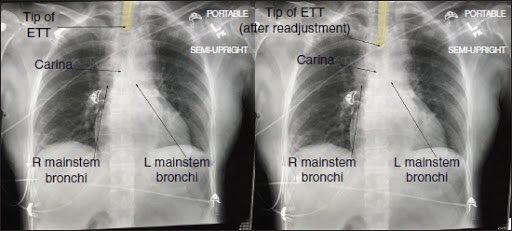
Placement: Post intubation you should get an X-ray. You want to make sure that the ETT is 5cm (+/-2) above the carina. This is a guideline ; ideal placement may vary. (Pic from Dr. Google)
You should also auscultate for bilat breath sounds & check an end tidal CO2 . ETCO2 measures the CO2 level at exhale. Normal is 35-45mmhg . ETCO2 monitoring detects apnea faster than respiration monitoring & O2 probes so they’re great for alarming if the circuit gets disconnected
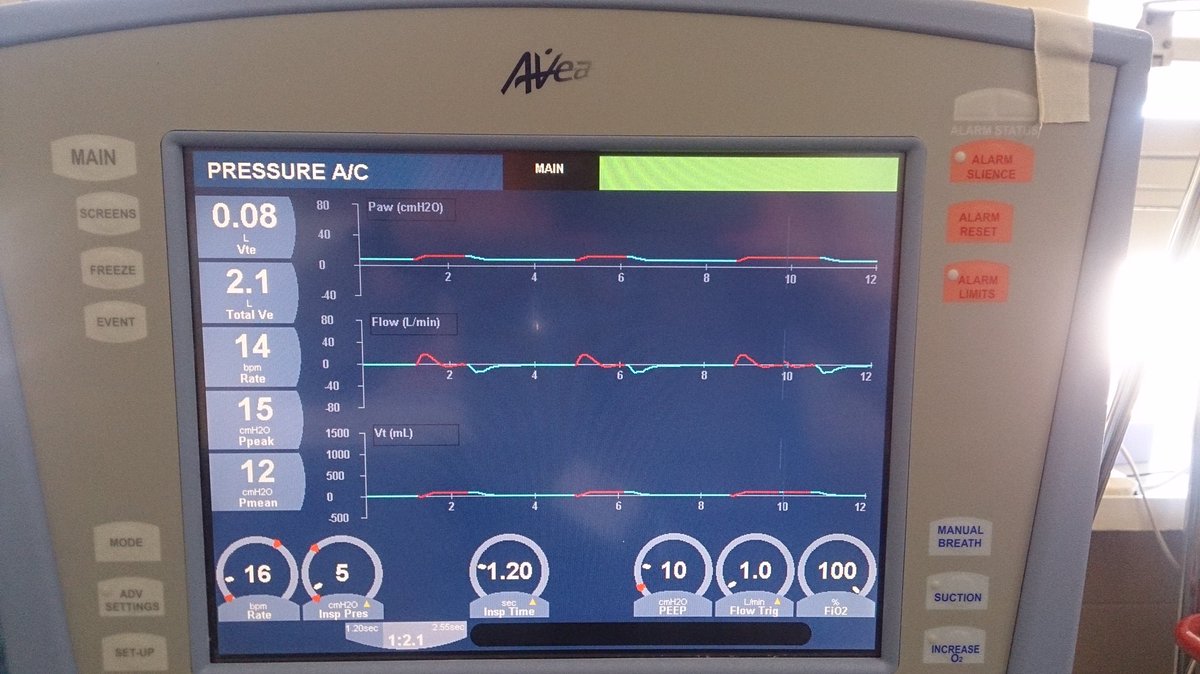
Waves: if you want a more in depth wave analysis , there are great YouTube video and I’ll retweet a few good sources . For basics sake, there will be two different colored waves. I believe it varies by vent brand so check with your RT
But for the Avea my hospital uses
Red wave : Machine triggered breath
Yellow: Patient triggered breath
Red wave : Machine triggered breath
Yellow: Patient triggered breath
There are a few vent modes but for COVID19 acute respiratory distress (ARDS) patients, they will more than likely be set to AC assist control mode. That’s the highest level of support where the machine controls the full breath.
You set Respiration Rate (RR), Tidal Volume (Vt), PEEP (positive end expiratory pressure), and FiO2 (concentration of O2, Room air is 21%). Now let’s break it down
Respiration Rate (RR): number of breaths you are administering to the patient. If ABG comes back respiratory alkolotic , team may consider lowering RR. If it’s Respiratory Acidosis, they may consider increasing RR.
Tidal Volume (Vt): volume delivered w/each breath. Based on ideal weight. Too high? Can create a pneumothorax.
PEEP: keeps the alveoli open at end expiration so that there is a greater surface area for gas exchange to occur. It recruits collapsing alveoli&makes them happy again. It’s a way to increase oxygenation w/o increasing FiO2. It’s important in ARDS patient who need that extra oomf
Peak Inspiratory Pressure (PIP): how much pressure it takes to deliver tidal volume. It’s a measurement of lung compliance. Lower PIP shows good lung compliance, higher PIP shows more pressure is needed to force the lungs to take in that volume.
Refer to your hospital policy, but where I’m at, every time a vent setting is changed, and ABG is drawn 1-2 hours after to determine response.
Alarms:
Circuit disconnect: pt disconnected from vent, if you can see where they popped off or where tubing came dislodged, reconnect them. If you can’t find it quickly by tracing the tubing, bag patient and call for back up.
Circuit disconnect: pt disconnected from vent, if you can see where they popped off or where tubing came dislodged, reconnect them. If you can’t find it quickly by tracing the tubing, bag patient and call for back up.
Alarms:
High pressure: Tubing is linked, pt needs to be suctioned (secretions are blocking the air passage), pt is biting ETT (place bite block and check sedation ), or pt is coughing
Low pressure: listen for cuff leak, check lines for disconnect
High pressure: Tubing is linked, pt needs to be suctioned (secretions are blocking the air passage), pt is biting ETT (place bite block and check sedation ), or pt is coughing
Low pressure: listen for cuff leak, check lines for disconnect
Sedation: Depending on how sick the patient is may influence what level of sedation a provider may want. If they want vent synchrony , they may order propofol drip. It’s short acting and easy to titrate to get the right level of sedation.
Bc it’s so short acting,you need to keep an eye on your bottle to make sure you don’t run dry. It can also cause hypotension so may need to add levo to keep the bp within goal. Tubing should be vented&changed q12 bc it has lipids which makes it an environment for microgrowth
Fentanyl is also a growing popular option. Some patients only need fentanyl drip to be synchronous with the vent but not completely knocked out. I.e great option for patients who are calmer and who can handle being awake while intubated without fighting the
machine (still maintains comfort & can be bolused for better control of the pt starts overbreathing too much).
Now, if a patient is in a lot of distress,they may need to be paralyzed.This should only be done by trained ICU nurses bc of the complex medications & monitoring needed
Now, if a patient is in a lot of distress,they may need to be paralyzed.This should only be done by trained ICU nurses bc of the complex medications & monitoring needed
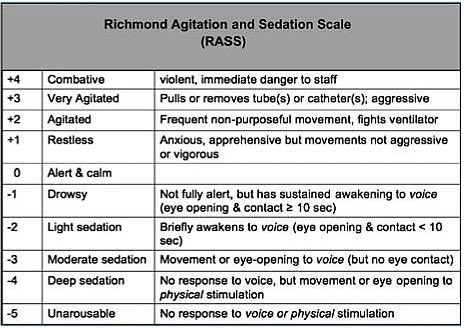
There are sedation scales that help guide medication titration. We use the Richman Agitation Sedation Scale (RASS) but there are others. Providers should set a score / parameters to guide your practice. EX: they want Pt to have a RASS of -3/-4 with complete vent synchrony
Suctioning: make sure you have the in like suction hooked up to the wall as well as a yankeur available at all times. We havent really been having in line secretions with these COVID19 patients but a lot of vented pts need q2-q4 suctioning . Pre oxygenate the pt.
There should be a oxygenate or suction button on the vent. The suction button will also silence alarms for 2 minutes (suctioning creates pressure ) . Make sure when you leave the room that the alarms are not still silenced!!!
Advance the in line catheter down the ETT until you elicit a cough (depending on sedation level of pt there may be no cough) . Start retracting the line while applying suction by holding your thumb down on the suction thing).
(Suctioning continues): Assess patient tolerance my monitoring their Pulse ox, blood pressure, and HR. Pt may require a break before you go back down for more secretions. Keep pt hyperoxygenated until sat returns to baseline
OG tube: Vented pts often have an OG tube placed for medication and nutrition. If you have never placed one before, please discuss with your manager about if you guys are going to be expected to be trained on placement.
One more point about the screen! The main screen should have two areas of readings. One for what the machine is set to, and one set of what the patient is actually doing
I think the most common layout is vent settings on the bottom and pt readings on side or on top . Once again, check with your RT (They are GOLDMINES of info) to clarify
If anyone else has any tips , tricks, or extra basic info to add to this thread DO IT UP
Also special shout out to @reepRN for proof reading to make sure I was making any sense after a long day of work

 Read on Twitter
Read on Twitter