After a week of self-isolation (with presumed mild COVID  https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">) reading just a few of the astonishing number of #SARSCoV2 & #COVID19 papers/pre-prints in between doses of paracetamol... Some thoughts and questions about what we know so far about COVID19 #immunology. 1/12
https://abs.twimg.com/emoji/v2/... draggable="false" alt="🤒" title="Face with thermometer" aria-label="Emoji: Face with thermometer">) reading just a few of the astonishing number of #SARSCoV2 & #COVID19 papers/pre-prints in between doses of paracetamol... Some thoughts and questions about what we know so far about COVID19 #immunology. 1/12
The big questions (IMO): does an aberrant immune response contribute to bad clinical outcomes? What is the nature of this immunopathological response? And conversely, what is a protective immune response to #SARSCoV2? 2/12
Inflammatory cytokines eg IL6, TNF correlate with severity/ARDS. IL10, chemokines also up. High admission IL6 predicts bad outcomes. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)30183-5/fulltext,">https://www.thelancet.com/journals/... https://academic.oup.com/cid/advance-article/doi/10.1093/cid/ciaa272/5807944.">https://academic.oup.com/cid/advan... What cells drive #CytokineStorm? Does it cause deterioration or is it a bystander phenotype? 3/12
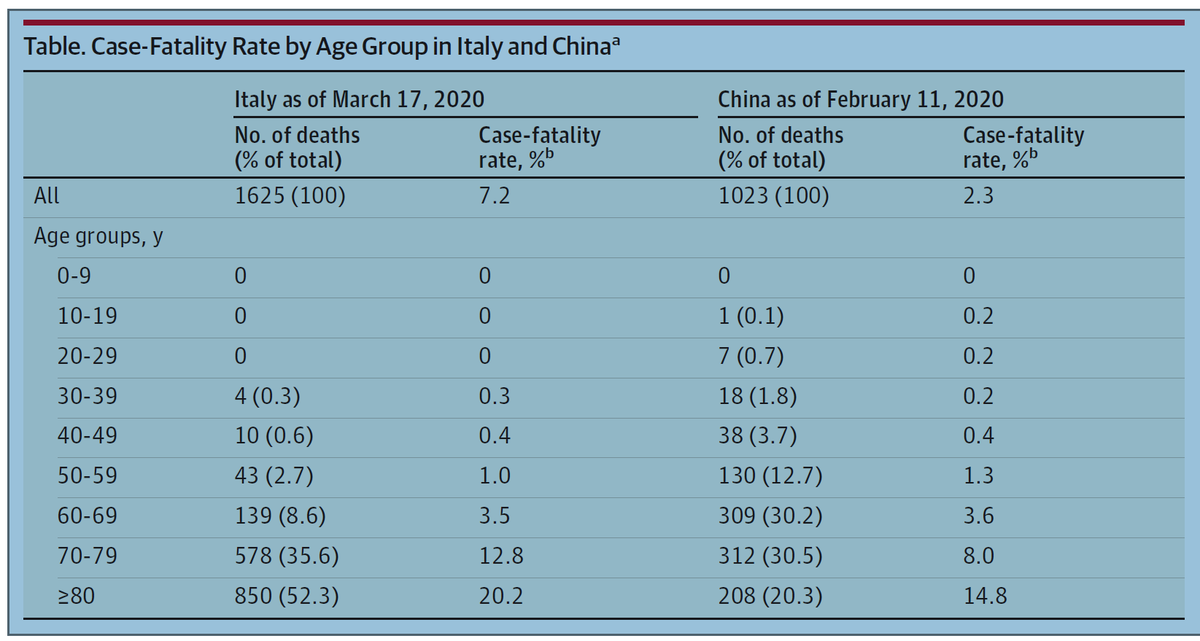
Outcomes for #COVID19 are markedly poorer in older adults (Onder et al, JAMA). If bad outcomes are driven by immunopathology/cytokine storming - what causes this? Related to immune senescence? Antibody or TCR cross-reactivity due to prior exposure to other CoVs? 4/12
IL-6R blockade, tocilizumab, is the big news in host-directed therapy (prelim results from China http://www.chinaxiv.org/abs/202003.00026)">https://www.chinaxiv.org/abs/20200... & going into trials https://www.roche.com/media/releases/med-cor-2020-03-24.htm.">https://www.roche.com/media/rel... Interested in whether colleagues are discussing other cytokine blockades (antiTNF, anti-IL1) for #COVID19? 5/12
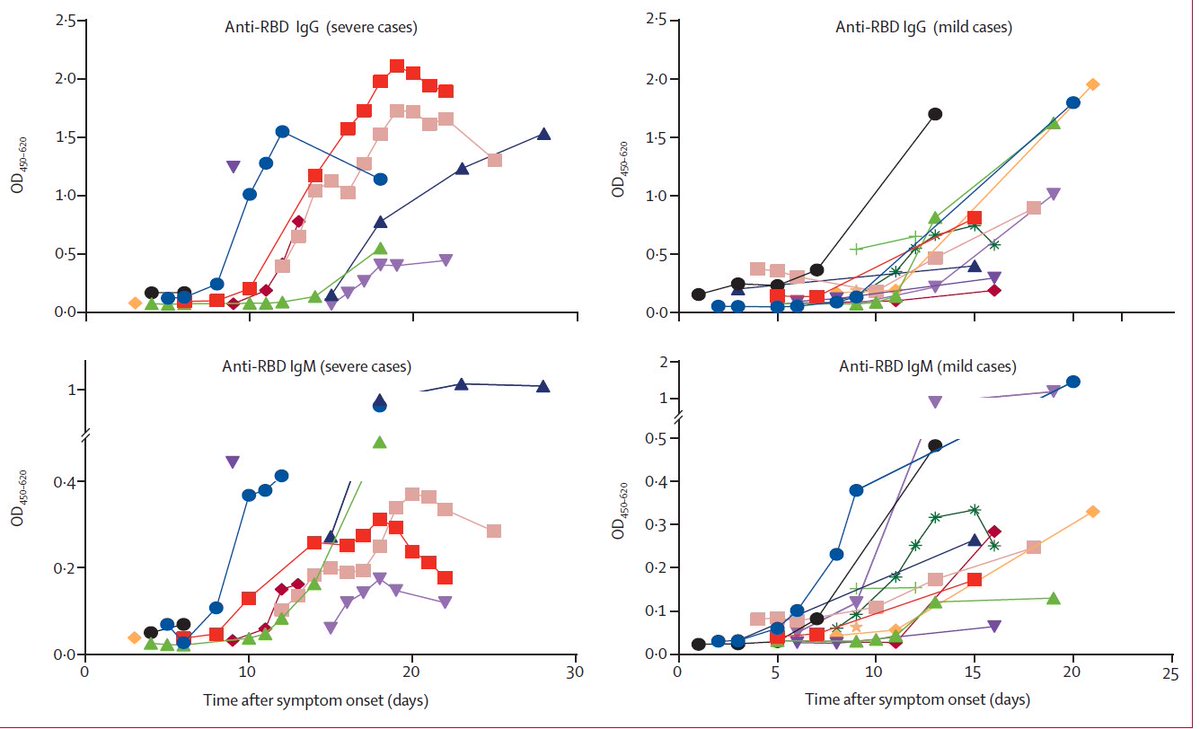
Pts with both mild & severe #COVID19 generate antibody responses by day 10 (To et al, Lancet ID). Prelim data suggest convalescent sera has therapeutic benefit https://jamanetwork.com/journals/jama/fullarticle/2763983.">https://jamanetwork.com/journals/... Is antibody protective? Why doesn& #39;t it protect in severe cases who have reasonable titres? 6/12
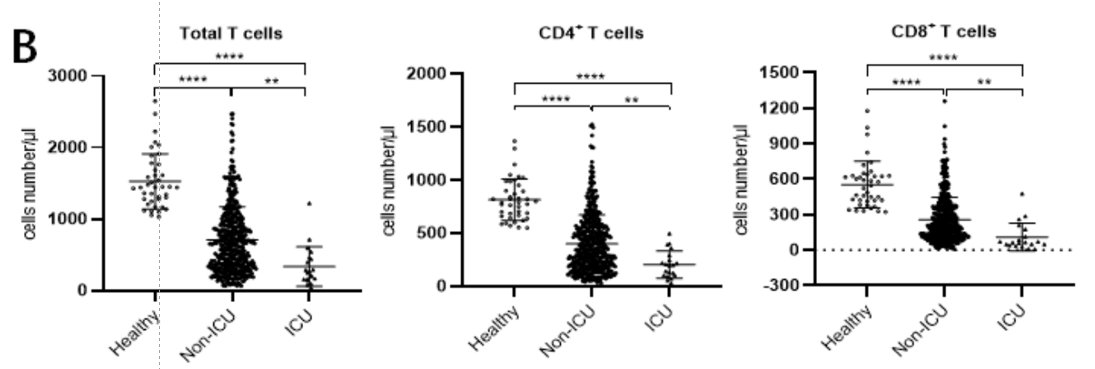
Lymphopenia marks and predicts severe disease. Total T-cells, CD4s and CD8s are all depleted in #COVID19 (Wu et al, JAMA Int Med; Diao et al preprint - https://www.medrxiv.org/content/10.1101/2020.02.18.20024364v1.full.pdf+html).">https://www.medrxiv.org/content/1... What is happening to the T-cells? 7/12
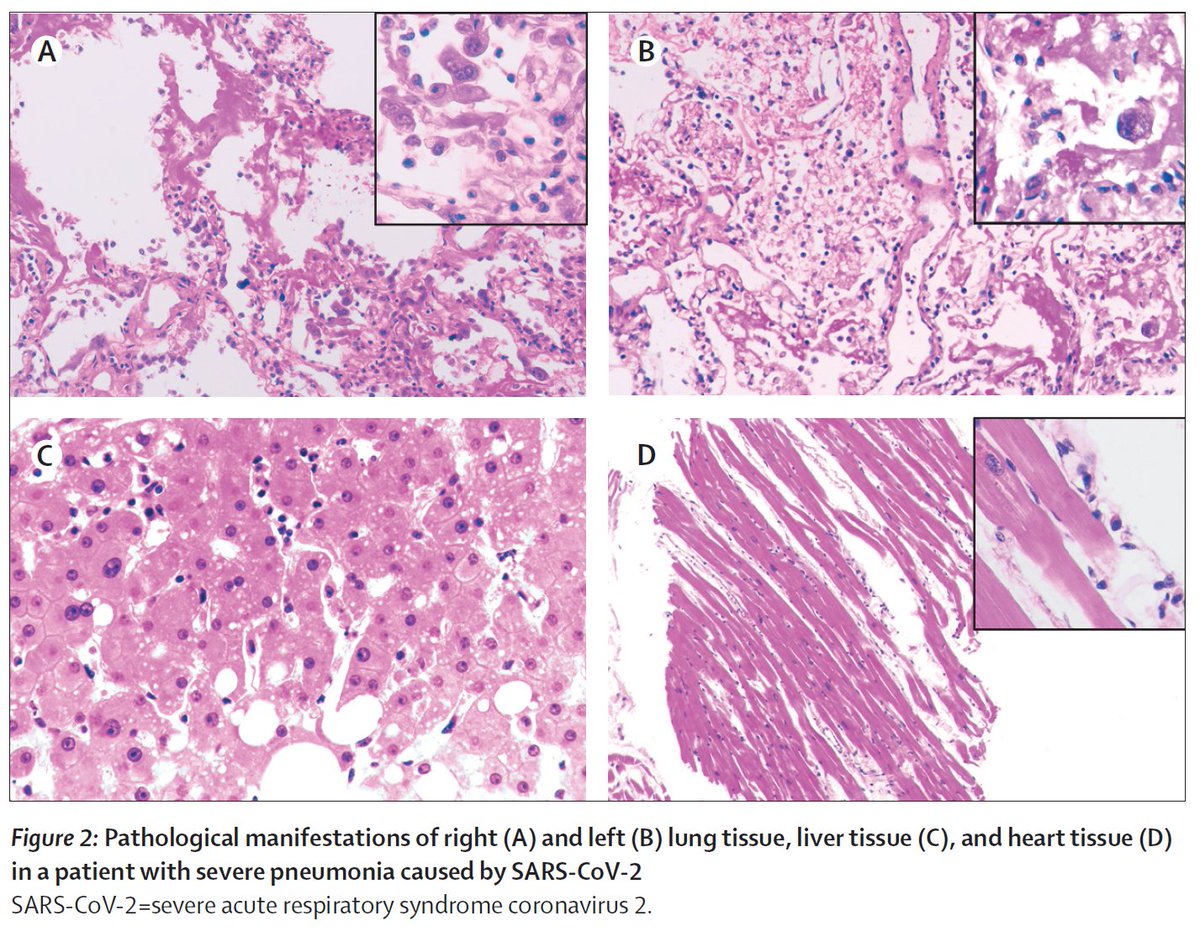
Are T-cells being & #39;consumed& #39; at the site of disease? Histopath of COVID19 lung shows lymphocyte infiltration - https://www.thelancet.com/journals/lancet/article/PIIS2213-2600(20)30076-X/fulltext.">https://www.thelancet.com/journals/... scSeq of BAL cells found clonally expanded CD8s in mild #COVID19 & proliferating T-cells in severe cases - https://doi.org/10.1101/2020.02.23.20026690">https://doi.org/10.1101/2... 8/12
Can we learn from the immune responses of asymptomatic individuals & children (who have asymptomatic or mild disease in the vast majority of cases) to discern what a protective immune response to #SARSCoV2 is? 9/12
Children generally do not develop lymphopenia with COVID-19 (Lu et al, NEJM). A small cohort of mildly symptomatic paediatric pts had detectable Th17-type cytokines (IL-6/IL-17F/IL-22) early in their disease course, in the absence of other cytokines (Xu et al, Nat Med). 10/12
Do IFN responses contribute to protection against #SARSCoV2? Early in vitro work suggests a muted IFN response, with supporting evidence in an animal model - https://www.biorxiv.org/content/10.1101/2020.03.24.004655v1">https://www.biorxiv.org/content/1... 11/12
Interested to hear thoughts of colleagues and the wider community. Future work in stratified populations including recovered individuals and those with mild #COVID19 disease will be key. 12/12
@innate2adaptive @gpollara @jamimmunology @CurlyJungleJake @JerryT88
@innate2adaptive @gpollara @jamimmunology @CurlyJungleJake @JerryT88

 Read on Twitter
Read on Twitter