The lack of clinical COVID19 cases in children is odd. Understanding why will be essential in deciding which social interventions are most useful. We discussed this alongside a modeling analysis here: https://dash.harvard.edu/handle/1/42639493
https://dash.harvard.edu/handle/1/... href="https://twitter.com/DrDJHaw">@DrDJHaw @BillHanage @CJEMetcalf @michaelmina_lab
We propose 4 possible explanations for the lack of cases in children:
1) Kids haven’t been making as many contacts as normal. This may contribute, but probably isn’t the only factor: https://www.medrxiv.org/content/10.1101/2020.03.19.20039107v1">https://www.medrxiv.org/content/1...
1) Kids haven’t been making as many contacts as normal. This may contribute, but probably isn’t the only factor: https://www.medrxiv.org/content/10.1101/2020.03.19.20039107v1">https://www.medrxiv.org/content/1...
2) Children are less susceptible to *infection* or adults are more susceptible. Seems unlikely now, given secondary attack rates from contact tracing, though conflicting findings: https://www.medrxiv.org/content/10.1101/2020.03.03.20028423v2">https://www.medrxiv.org/content/1... + previous
3) There are many asymptomatic children out there not being reported. Seems obvious and likely but contradicts early WHO reports.
4) *Transmissibility* increases with age possibly through increased frequency/severity of symptoms (see below by Davies et al). We felt this was a key point – transmission models with age-dependent *susceptibility* are different to those with age-dependent *transmissibility*
We conclude that 3) and/or 4) are the most likely. Which scenario we’re in has profound implications for control measures, as different ages may be contributing hugely different amounts to overall transmission. We need contact tracing with children as the index case to find out:
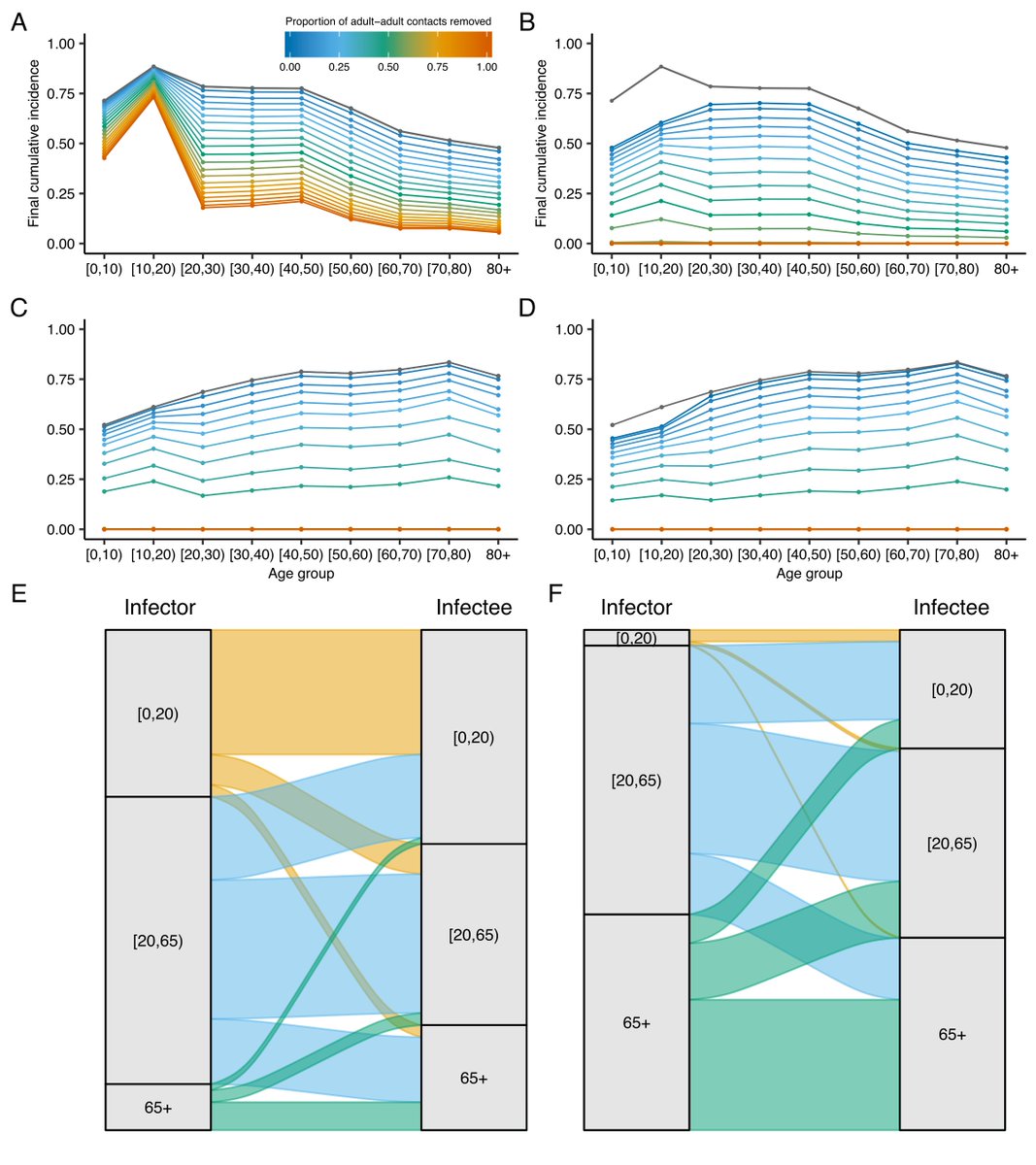
(Top row shows epidemic final size with uniform age-dependent transmissibility, bottom is with increasing transmissibility with age. LHS shows no school closures, RHS shows with school closures)
This is a less timely piece than we wanted (mysterious issues getting this on preprint servers then stuck in unsuccessful review), and others have taken a much more thorough and data-driven approach to this issue:
@rozeggo and @_nickdavies’ modeling analysis. Looks like we converged on the same train of thought, but they took it to a much more satisfying conclusion and I really like their analysis (they formally fit to data): https://twitter.com/rozeggo/status/1242606769047814144">https://twitter.com/rozeggo/s...
@akelvinlab and Scott Halperin have discussed a recent observational cohort here: https://twitter.com/akelvinlab/status/1243161833399365632">https://twitter.com/akelvinla...
As ever in this unusual, time-critical period, this is not yet peer reviewed.

 Read on Twitter
Read on Twitter