It is perplexing to see that the article ignores tactics of Japan, where R0 of COVID-19 is clearly lower. The purpose of this thread is to search for reasons why Japan has been successful. 1/
https://science.sciencemag.org/content/367/6484/1287">https://science.sciencemag.org/content/3...
https://science.sciencemag.org/content/367/6484/1287">https://science.sciencemag.org/content/3...
Disclaimer: I am a cell biologist studying mitosis, and not an expert of infectious disease. I& #39;ve gathered most information is from internet. It would be great if experts @PaulBieniasz, @danmucida, @VirusesImmunity & others . 2/
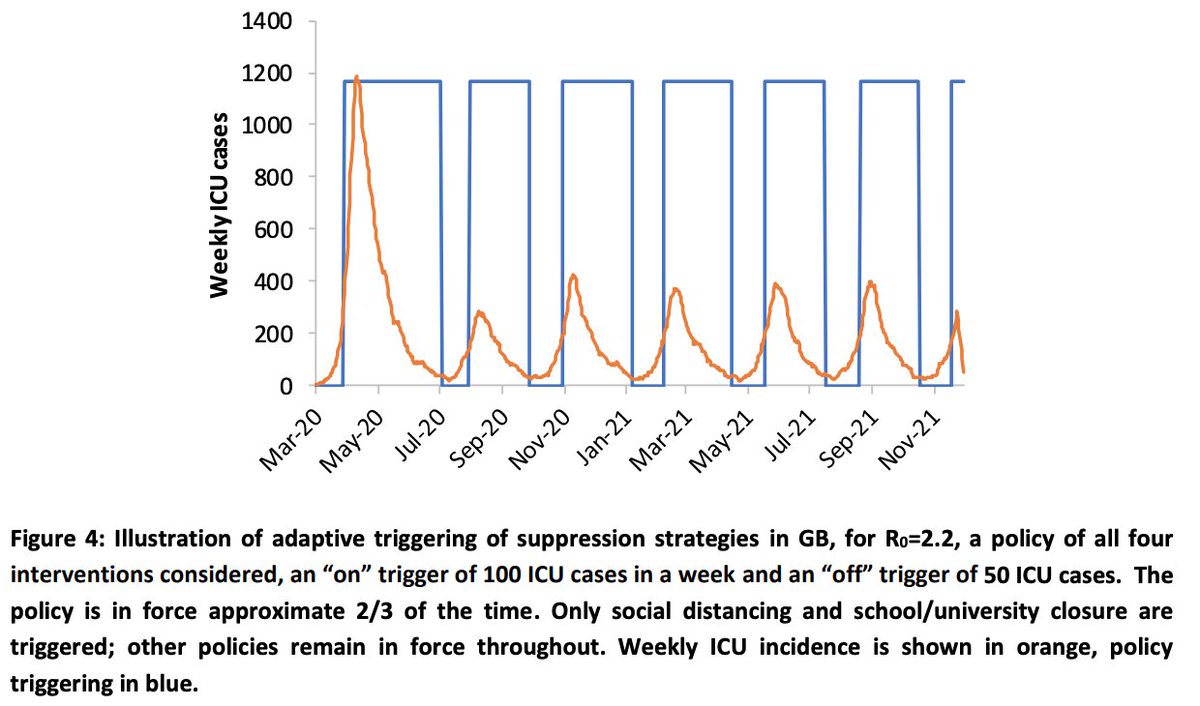
Many of you are now familiar with a simulation analysis of Fergusson et al, indicating that mitigation (R0<1) is not sufficient to prevent hospital overload, while suppression (R0<1) would take years to gain herd immunity until we get vaccines. 3/
https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf">https://www.imperial.ac.uk/media/imp...
https://www.imperial.ac.uk/media/imperial-college/medicine/sph/ide/gida-fellowships/Imperial-College-COVID19-NPI-modelling-16-03-2020.pdf">https://www.imperial.ac.uk/media/imp...
The future of next 2 years predicted by Fergusson is depressing, as it demands strong restriction of school/university and business to accomplish R<1. In Japan, so far R0≅1 has been accomplished with volunteer-based cancellations of large-scale events, and school closures. 4/
Although most sports and music events have been cancelled in Japan, a large majority of people go outside and work, and restaurants are open. Schools are currently spring break period, but they are trying to open in April. 5/
If the R0≅1 can be maintained with this minimum restrain, and if the R01 can be naturally reduced when humid summer arrives, there is a reasonable chance that the society can maintain good activities without risking hospital overload. 6/ https://www.accuweather.com/en/health-wellness/new-study-says-high-temperature-and-high-relative-humidity-significantly-reduce-spread-of-covid-19/703418">https://www.accuweather.com/en/health...
Remember that a lot of tourists from China visited Japan during Chinese New Year. There was also a case of Diamond Princess. However, they did not trigger catastrophe. So how did Japanese do? 7/
The Government of Japan, Cluster Response Team of Ministry of Health, Labour and Welfare (MHLW) has stated The three pillars of Japan& #39;s strategy:
https://www.mhlw.go.jp/content/10900000/000608425.pdf
8/">https://www.mhlw.go.jp/content/1...
https://www.mhlw.go.jp/content/10900000/000608425.pdf
8/">https://www.mhlw.go.jp/content/1...
1) early detection of and early response to clusters
2)early patient diagnosis and enhancement of intensive care and the securing of a medical service system for the severely ill
3) behavior modification of citizens
9/
2)early patient diagnosis and enhancement of intensive care and the securing of a medical service system for the severely ill
3) behavior modification of citizens
9/
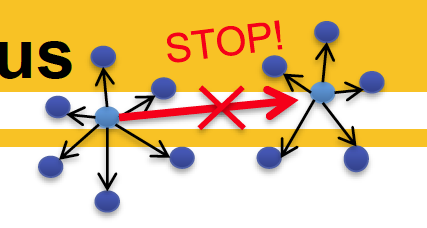
The underlying principle is laid out in this handout by MHLW.
“The important thing is to minimize the spread of infection in the country by preventing one cluster of patients from creating another cluster.”
10/
https://www.mhlw.go.jp/content/10200000/000603320.pdf">https://www.mhlw.go.jp/content/1...
“The important thing is to minimize the spread of infection in the country by preventing one cluster of patients from creating another cluster.”
10/
https://www.mhlw.go.jp/content/10200000/000603320.pdf">https://www.mhlw.go.jp/content/1...
Cluster Response Team of Ministry of Health, lead by Hiroshi Nishiura, Prof at Hokkaido Univ. and an expert of mathematical modeling of infectious disease, defined characteristics of the transmission rout as:
11/
11/
"1) So far, approximately 80% of the confirmed infection cases in Japan have not transmitted the infection to others."
12/
12/
"2) Meanwhile, cases have been reported where a single infected patient has transmitted the infection to multiple persons in areas such as athletic gyms, houseboats, buffet style meals, mahjong rooms, guest houses at ski resorts, and air-tight provisional tents."
13/
13/
Supporting data from Nishiura are available in this preprint.
“The odds 44 that a primary case transmitted COVID-19 in a closed environment was 18.7 times greater compared to an open-air environment (95% confidence interval [CI]: 6.0, 57.9). “ 14/
https://www.medrxiv.org/content/10.1101/2020.02.28.20029272v1.full.pdf">https://www.medrxiv.org/content/1...
“The odds 44 that a primary case transmitted COVID-19 in a closed environment was 18.7 times greater compared to an open-air environment (95% confidence interval [CI]: 6.0, 57.9). “ 14/
https://www.medrxiv.org/content/10.1101/2020.02.28.20029272v1.full.pdf">https://www.medrxiv.org/content/1...
So, the team set the priority to suppress super-spreading events, and urges people to avoid places where the following three conditions were met simultaneously:
15/
15/
1) closed space with poor ventilation
2) crowded with many people
3) conversations and vocalization in close proximity (within arm& #39;s reach of one another)
16/
2) crowded with many people
3) conversations and vocalization in close proximity (within arm& #39;s reach of one another)
16/
It is worth noting that following this advice, the government even encourage people to go outside. An opposite of what is happening in NYC.
https://twitter.com/Kantei_Saigai/status/1240541777712443393
17/">https://twitter.com/Kantei_Sa...
https://twitter.com/Kantei_Saigai/status/1240541777712443393
17/">https://twitter.com/Kantei_Sa...
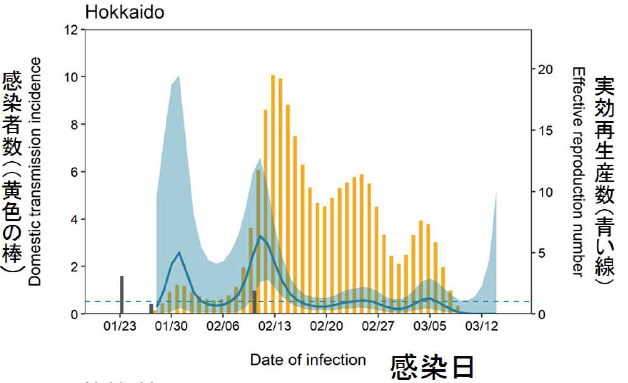
Now, as an example, I& #39;d like to explain a case in Hokkaido, where clusters of COVID-19 were detected from late January.
18/
18/
There was Sapporo Snow Festival held from 1/31 to 2/11, where 2M people visited, likely causing clustered infections at this period. A lot of closed, crowded temporal spaces without good ventilation where many tourists gathered, talked and ate foods were generated.
19/
19/
On 2/28, State of Emergency was declared in Hokkaido, after detecting 15 and 12 positive cases on 2/27 & 28, respectively. Total# was 66 at that point.
20/
20/
The mayor requested Hokkaido citizens to refrain from going outside during weekends. Public schools were closed from 2/28. Large-scale events were asked to be canceled.
https://www.nikkei.com/article/DGXMZO56188700Y0A220C2L41000/
21/">https://www.nikkei.com/article/D...
https://www.nikkei.com/article/DGXMZO56188700Y0A220C2L41000/
21/">https://www.nikkei.com/article/D...
Meanwhile, cluster Response Team of Ministry of Health, Labour and Welfare (MHLW), National Institute of Infectious Diseases (NIID) and local public health center worked together to isolate patients and their close contacts through PCR testing. 22/
Thanks to early detection and isolations of patients, a burst of infection in Hokkaido was successfully prevented, and now R0 is maintained below 1.
On March 18, the mayor of Hokkaido declared State of Emergency to be terminated next day as has initially planned. 23/
On March 18, the mayor of Hokkaido declared State of Emergency to be terminated next day as has initially planned. 23/
So how the team was able to successfully detect infected cases?
Population of Sapporo, capital of Hokkaido, is 2M. The size of Hokkaido is similar to Maine.
I& #39;d like to start with testing. 24/
Population of Sapporo, capital of Hokkaido, is 2M. The size of Hokkaido is similar to Maine.
I& #39;d like to start with testing. 24/
OK. Here comes the limit of max tweet numbers in a thread.
I& #39;ll take some break, and will continue the thread this later.
25/
I& #39;ll take some break, and will continue the thread this later.
25/
I& #39;m back. Please keep in mind that the strategy working for Japan may not be directly applicable to cities like NYC, which is facing hospital overloads. For us (New Yorkers), it is important now to do whatever possible to do to suppress the current burst of infections. 26/
What I am hoping to do here is to see if we can learn some hints for a long term solution for COVID-19 from Japan, which is apparently handling the situation relatively well so far.
27/
27/
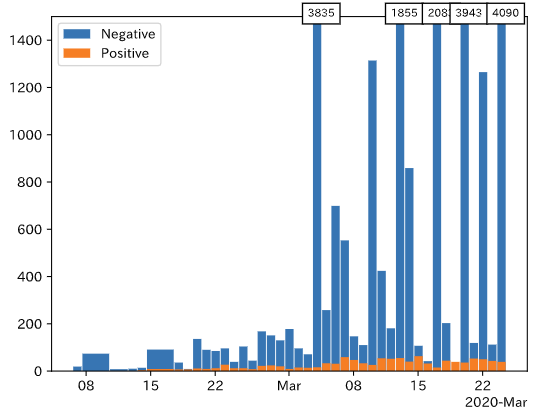
So, back to testing. I know that there has been some doubts on COVID-19 case counting in Japan due to low numbers of testing. I have limited information, but I can point out a few things. 28/
First, different countries are using different PCR protocols and primers to detect SAR-CoV-2. What I heard from my microbiologist friend in Japan is that NIID made great efforts to establish a reliable protocol, which is now being used in Japan.
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/laboratory-guidance
29/">https://www.who.int/emergenci...
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/laboratory-guidance
29/">https://www.who.int/emergenci...
Second, RT-PCR-based testing generates a lot of false negatives and also false positives. To effectively identify infected patients with limited resource, it is important to focus the testing on patients with high likelihood of COVID-19.
https://twitter.com/Dr_yandel/status/1232463168422567937
30/">https://twitter.com/Dr_yandel...
https://twitter.com/Dr_yandel/status/1232463168422567937
30/">https://twitter.com/Dr_yandel...
The symptoms to meet SARS-CoV-2 testing are: patients who have fever >37.5°C/respiratory symptoms & had a close contact history with an infected patient, visited or contacted with those who visited to high risk countries, or may have pneumonia requiring hospitalization. 31/
Then, after tests for influenza and other general infections come out negative, patients will get a PCR test for SARS-CoV-2/COVID-19. I don& #39;t know if this guideline has been broadly practiced, but this what MHLW has distributed.
https://www.mhlw.go.jp/content/000609467.pdf
32/">https://www.mhlw.go.jp/content/0...
https://www.mhlw.go.jp/content/000609467.pdf
32/">https://www.mhlw.go.jp/content/0...
Meanwhile, MHLW made a clear guideline for patients with suspicion of COVID-19 infection about when to call the designated consultation centers in each prefectures. This aimed to prevent people from rushing into hospitals with mild symptoms.
https://www.mhlw.go.jp/content/10200000/000603610.pdf
33/">https://www.mhlw.go.jp/content/1...
https://www.mhlw.go.jp/content/10200000/000603610.pdf
33/">https://www.mhlw.go.jp/content/1...
When the SARS-CoV-2 positive patients were identified, their contacted people are quickly noticed, and quarantined. Again, the key is how to effectively identify true infected patients with limited resources, and to prevent the spread from there. 34/
Third, I know that many Japanese journalists are always looking for bad news, and often they exaggerate. However, no news about hospital overload in Japan has been reported so far. As of 3/21, total deaths by COVID-19 are 35 and 60 in Japan and NYC, respectively. 35/
So, I highly doubt conspiracy theories, like Japan is suppressing COVID-19 cases to keep Tokyo Olympics alive. Priority was set to effectively detect infected patients, and this task was achieved without random broad testings in Japan.
36/
36/
I would like to end this thread by some cultural aspects that may have been helping Japan. These are pure speculation, but my microbiologist friend actually thinks that these factors may have been playing more important roles. 37/
Face masks. Some argue that face masks are only useful for infected patients not to spread viruses, but they are not effective for protection. Two issues about this. First, since asymptomatic patients are likely to be infectious, masks could help spread viruses from them. 38/
Second, we are asked not to touch our face, because mouth, nose, and eyes are major infection routes. So, why doesn& #39;t a mask help? However, the unfortunate practical reason why we discourage people from wearing masks is mainly to save masks for health care workers. 39/
In Japan, thanks to widespread severe allergies to cedar pollens, it has been ordinary for Japanese to wear masks. Although there are shortage in masks in Japan as well, people are hand-making them at home to survive allergy season. Many youtube instructions are available. 40/
Another cultural point is related to Ruth Benedict’s idea of Western guilt cultures and Japanese shame cultures. Few speaks in buses and trains in Japan. Cell phone talking is strictly discouraged. Many local habitual rules must be obeyed not to be ashamed in public. 41/
Even in Tokyo where trains are packed everyday, spreading of COVID-19 appears to have been suppressed since it was first detected on 1/24. As of 3/21, total COVID-19 cases in Tokyo are only 136 in the city with 10M. This is remarkable to me. 42/
Religious assemblies. Few Japanese “actively” engages in religious assemblies, except for funerals, weddings, and other special occasions. Even at these occasions, except for receptions, participants keep silence during ceremonies. 43/
In contrast, in Christian masses, participants actively engage singing and speaking inside churches. A lot of handshakes and hugging as well. In Japan, body touching is still not common. 44/
Finally, after COVID-19, I realized that to eat pieces of bread & pizza I must touch them with bare hands. In Japan, it is rare to use bare hands to eat foods generally except for sushi and some snacks. Many of snacks are individually wrapped like this photo. 45/
I wonder if these "no-contact" Japanese customs have evolved in relation to infectious diseases. I& #39;ve learned some history of infectious diseases in Europe and consequence of European invasions, but know very little about history of infectious diseases in Japan and Asia. 46/
The tactics taken in Japan may not be immediately useful in NYC, but may work for other cities where COVID-19 have not hit hard yet. There are many regions in US to protect. 47/
Importantly, Expert Meeting on the Novel Coronavirus Disease Control in Japan recognizes upcoming burdens, and requests government for further enforcement on the system to cope with COVID-19 cluster expansions. So we should keep an eye on the situation in Japan as well. 48/
So, here comes the end. Thanks for reading this long thread. Hope this is useful and gives food for thought. Small collective efforts can have significant impacts as this math calculation below demonstrates.
Stay safe!
https://twitter.com/HironoriFunabi1/status/1237010900718149633
End/49">https://twitter.com/HironoriF...
Stay safe!
https://twitter.com/HironoriFunabi1/status/1237010900718149633
End/49">https://twitter.com/HironoriF...
Here is a nice coverage by Washington Post on how Wakayama prefecture in Japan executed COVID-19 cluster identification. https://www.washingtonpost.com/world/asia_pacific/japan-coronavirus-wakayama/2020/03/22/02da83bc-65f5-11ea-8a8e-5c5336b32760_story.html">https://www.washingtonpost.com/world/asi...
I would like to add this fantastic Japanese site, which greatly clarified my understanding. It has more detailed explanations for why random testing & false positive are problematic, and why Japan needs to do better. Perhaps somebody can translate this. https://note.com/kyoshimine/n/n6bf078a369f9?fbclid=IwAR0mBg91aTotZ1kVDKPUv5lIkOKv7-qZwepTc_Mny-9hsgNhtMwyAneEWMU">https://note.com/kyoshimin...
Some are still pointing out low # testing. Here, left is total, right is daily test results in Japan. A large majority of test outcomes are still PCR negative, so increasing test # would not affect slope of the curve much.
https://oku.edu.mie-u.ac.jp/~okumura/python/COVID-19.html">https://oku.edu.mie-u.ac.jp/~okumura/...
https://oku.edu.mie-u.ac.jp/~okumura/python/COVID-19.html">https://oku.edu.mie-u.ac.jp/~okumura/...
This is an English translation of the Japanese site that I have mentioned above, #51 of my tweet. There are a lot more information and discussions. https://medium.com/@shotamiz/how-japan-is-combating-sars-cov-2-covid-19-83b7dd8d3f9">https://medium.com/@shotamiz...
The situation in Tokyo is alarming. A critical moment for Japan... https://stopcovid19.metro.tokyo.lg.jp/en ">https://stopcovid19.metro.tokyo.lg.jp/en"&...
I would like to place a link to this English translated version of NHK documentary here as well. The counter cluster team warns that despite past successful efforts to suppress COVID-19 in Japan, it won& #39;t be sustainable without further additional actions. https://www3.nhk.or.jp/nhkworld/en/ondemand/video/5001289/">https://www3.nhk.or.jp/nhkworld/...

 Read on Twitter
Read on Twitter
![Supporting data from Nishiura are available in this preprint. “The odds 44 that a primary case transmitted COVID-19 in a closed environment was 18.7 times greater compared to an open-air environment (95% confidence interval [CI]: 6.0, 57.9). “ 14/ https://www.medrxiv.org/content/1... Supporting data from Nishiura are available in this preprint. “The odds 44 that a primary case transmitted COVID-19 in a closed environment was 18.7 times greater compared to an open-air environment (95% confidence interval [CI]: 6.0, 57.9). “ 14/ https://www.medrxiv.org/content/1...](https://pbs.twimg.com/media/ETt3xf9XQAADOwP.png)