A #hemetwitter #tweetorial
DIC.
In med school, we were taught that DIC stood for disseminated intravascular coagulation.
Or...
Death. Is. Coming.
1/n
DIC.
In med school, we were taught that DIC stood for disseminated intravascular coagulation.
Or...
Death. Is. Coming.
1/n
This is severe and may be a bit hyperbolic.
But DIC is nothing to mess around with.
So what is it exactly?
At its core, DIC is coagulation gone rogue.
2/n
But DIC is nothing to mess around with.
So what is it exactly?
At its core, DIC is coagulation gone rogue.
2/n
For those that aren& #39;t coagulation nerds, a quick primer.
Following blood vessel injury, primary hemostasis occurs involving collagen, VWF, platelets.
Secondary hemostasis is comprised of the intrinsic (PTT) and extrinsic (PT) pathways which converge at the common pathway.
3/n
Following blood vessel injury, primary hemostasis occurs involving collagen, VWF, platelets.
Secondary hemostasis is comprised of the intrinsic (PTT) and extrinsic (PT) pathways which converge at the common pathway.
3/n
The common pathway generates thrombin, which converts fibrinogen to fibrin.
So where does this go wrong?
First, it is important to note that DIC is not an independent disorder. It is ALWAYS a complication of another issue.
4/n
So where does this go wrong?
First, it is important to note that DIC is not an independent disorder. It is ALWAYS a complication of another issue.
4/n
The 1st report of DIC was back in 1834 by Dupuy who described what occurred when brain material was injected intravenously into animals. Yikes.
The animals died quickly and widespread clots were found throughout their bodies.
Glad I didn& #39;t have to do those experiments..
5/n
The animals died quickly and widespread clots were found throughout their bodies.
Glad I didn& #39;t have to do those experiments..
5/n
Causes of DIC in people include:
-Infections (occurring in up to 30% of septic pts)
-Polytrauma
-Scary OB stuff (retained fetus, placental abruption, amniotic fluid embolism)
-Malignancy
-Vascular malformations
-Burns
-Snake bites
-Hopefully not brain injection
6/n
-Infections (occurring in up to 30% of septic pts)
-Polytrauma
-Scary OB stuff (retained fetus, placental abruption, amniotic fluid embolism)
-Malignancy
-Vascular malformations
-Burns
-Snake bites
-Hopefully not brain injection
6/n
All involve systemic inflammatory responses, a crucial factor in the pathogenesis of DIC.
The initiator of coagulation in DIC is tissue factor (TF), an extrinsic pathway component. TF is on the surface of many cell types but generally not in contact with circulating blood.
7/n
The initiator of coagulation in DIC is tissue factor (TF), an extrinsic pathway component. TF is on the surface of many cell types but generally not in contact with circulating blood.
7/n
TF is normally exposed after vascular damage but is released in response to cytokines, TNF, and endotoxin.
It is abundant in tissue of lung, brain and placenta, explaining DIC in response to polytrauma (and IV brain injection).
8/n
It is abundant in tissue of lung, brain and placenta, explaining DIC in response to polytrauma (and IV brain injection).
8/n
Platelet activation (also 2/2 inflammation) greatly facilitates coagulation activation.  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">interaction btw platelets/vessel wall can lead to a thrombotic microangiopathy in some pts!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">interaction btw platelets/vessel wall can lead to a thrombotic microangiopathy in some pts!
VWF is involved as an acute phase reactant and ultra large (UL) multimers are released.
9/n
VWF is involved as an acute phase reactant and ultra large (UL) multimers are released.
9/n
This is why pts with severe inflammatory responses frequently have  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> ADAMTS13!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> ADAMTS13!
ADAMTS13 is an important protease responsible for cleaving VWF. https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> UL VWF leads to
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> UL VWF leads to  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">
consumption of ADAMTS13.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> ADAMTS13 has been shown to be as predictive of mortality as APACHE
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> ADAMTS13 has been shown to be as predictive of mortality as APACHE  https://abs.twimg.com/emoji/v2/... draggable="false" alt="😳" title="Errötetes Gesicht" aria-label="Emoji: Errötetes Gesicht">
https://abs.twimg.com/emoji/v2/... draggable="false" alt="😳" title="Errötetes Gesicht" aria-label="Emoji: Errötetes Gesicht">
10/n
ADAMTS13 is an important protease responsible for cleaving VWF.
consumption of ADAMTS13.
10/n
Normally, coagulation is balanced by anticoagulants (proteins C,S, TFPI and AT). In DIC these controls are dysfunctional, allowing unchecked activation.
Fibrinolysis is also inhibited due to https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">levels of PAI-1 (an inhibitor of plasmin, the key factor in fibrinolysis)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">levels of PAI-1 (an inhibitor of plasmin, the key factor in fibrinolysis)
11/n
Fibrinolysis is also inhibited due to
11/n
Evidence now suggests that cell free DNA, extracellular histones and DNA binding proteins play a key role, contributing to NETosis which is highly procoagulant.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">plasma levels of DNA-histone complexes and double-stranded DNA correlate with DIC severity.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">plasma levels of DNA-histone complexes and double-stranded DNA correlate with DIC severity.
12/n
12/n
So..
Fibrin clots in circulation https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">trap platelets to make bigger clots
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">trap platelets to make bigger clots  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> micro and macro-vascular thrombosis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> micro and macro-vascular thrombosis
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> ischemia, inadequate perfusion, and end organ damage.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> ischemia, inadequate perfusion, and end organ damage.
Diagnosis of DIC is based on laboratory testing in the right clinical context.
13/n
Fibrin clots in circulation
Diagnosis of DIC is based on laboratory testing in the right clinical context.
13/n
Lab criteria for DIC include
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">PT, PTT (factor consumption)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">PT, PTT (factor consumption)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">platelets (consumption)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten">platelets (consumption)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> fibrinogen (consumption)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> fibrinogen (consumption)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> D-dimer or fibrin degradation products (formed during fibrin formation and subsequent degradation)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben"> D-dimer or fibrin degradation products (formed during fibrin formation and subsequent degradation)
ISTH& #39;s helpful scoring algorithm
https://cdn.ymaws.com/www.isth.org/resource/group/1188b45f-809f-4e2d-b3ef-c6836c51440b/official_communications/definitionofdic.pdf
14/n">https://cdn.ymaws.com/www.isth....
ISTH& #39;s helpful scoring algorithm
https://cdn.ymaws.com/www.isth.org/resource/group/1188b45f-809f-4e2d-b3ef-c6836c51440b/official_communications/definitionofdic.pdf
14/n">https://cdn.ymaws.com/www.isth....
It& #39;s important to recognize that fibrinogen is an acute phase reactant and given inflammation may be  https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">.
One study found that only 8.6% of pts with DIC have https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> fibrinogen and recommended using a fibrinogen/CRP ratio instead.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬇️" title="Pfeil nach unten" aria-label="Emoji: Pfeil nach unten"> fibrinogen and recommended using a fibrinogen/CRP ratio instead.
https://www-karger-com.proxy.lib.umich.edu/Article/Pdf/96786
15/n">https://www-karger-com.proxy.lib.umich.edu/Article/P...
One study found that only 8.6% of pts with DIC have
https://www-karger-com.proxy.lib.umich.edu/Article/Pdf/96786
15/n">https://www-karger-com.proxy.lib.umich.edu/Article/P...
The ISTH score (which uses fibrinogen) has NPV and PPV of ~95% and is predictive of mortality with a diagnosis of overt DIC doubling risk.
Given fibrin deposition then factor consumption, patients with DIC are at risk for bleeding and thrombosis.
So how do we treat?
16/n
Given fibrin deposition then factor consumption, patients with DIC are at risk for bleeding and thrombosis.
So how do we treat?
16/n
Tx of DIC is focused on treating the UNDERLYING problem.
Optimal tx of coagulation derangements is controversial.
Heparin blocks experimental DIC but clinical evidence is mixed.
Activated protein C was tried due to its anti-inflammatory and anticoagulant properties..
17/n
Optimal tx of coagulation derangements is controversial.
Heparin blocks experimental DIC but clinical evidence is mixed.
Activated protein C was tried due to its anti-inflammatory and anticoagulant properties..
17/n
Results were disappointing. Data on AT has been mixed although a few meta analyses have shown some survival benefit.
Thrombomodulin (TM) has also been studied. TM is a cofactor in the activation of protein C but more importantly has anti-thrombotic, anti-inflammatory..
18/n
Thrombomodulin (TM) has also been studied. TM is a cofactor in the activation of protein C but more importantly has anti-thrombotic, anti-inflammatory..
18/n
and cyto-protective properties.
Trial data has been favorable with decreased mortality but has not been statistically significant.
Recombinant ADAMTS13 is also being explored.
Antifibrinolytics and PCCs are generally avoided due to risk of thrombosis.
19/n
Trial data has been favorable with decreased mortality but has not been statistically significant.
Recombinant ADAMTS13 is also being explored.
Antifibrinolytics and PCCs are generally avoided due to risk of thrombosis.
19/n
Tx is indicated for symptomatic patients with bleeding or thrombosis.
Tx should not be withheld due to fear of "feeding the fire." But the goal should not be to normalize laboratory values. However, most groups agree on a minimum platelet threshold of 10-20K.
20/n
Tx should not be withheld due to fear of "feeding the fire." But the goal should not be to normalize laboratory values. However, most groups agree on a minimum platelet threshold of 10-20K.
20/n
Many pts with vascular malformations have chronic DIC for years.
For these pts, I can assure you, death is NOT coming.
For severe sepsis, trauma, burns, mortality rates are 40-80% and https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">with patient age and severity of derangements.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⬆️" title="Pfeil nach oben" aria-label="Emoji: Pfeil nach oben">with patient age and severity of derangements.
Yikes. Scary stuff.
21/fin
For these pts, I can assure you, death is NOT coming.
For severe sepsis, trauma, burns, mortality rates are 40-80% and
Yikes. Scary stuff.
21/fin

 Read on Twitter
Read on Twitter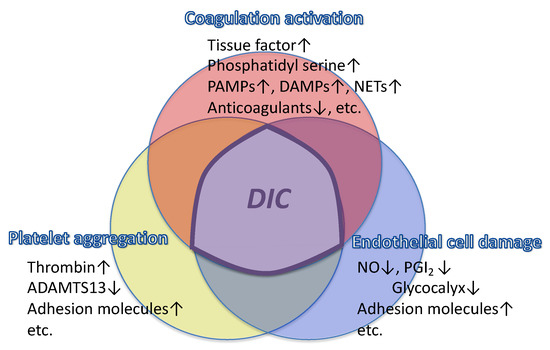 trap platelets to make bigger clots https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> micro and macro-vascular thrombosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> ischemia, inadequate perfusion, and end organ damage. Diagnosis of DIC is based on laboratory testing in the right clinical context.13/n" title="So..Fibrin clots in circulationhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">trap platelets to make bigger clots https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> micro and macro-vascular thrombosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> ischemia, inadequate perfusion, and end organ damage. Diagnosis of DIC is based on laboratory testing in the right clinical context.13/n" class="img-responsive" style="max-width:100%;"/>
trap platelets to make bigger clots https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> micro and macro-vascular thrombosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> ischemia, inadequate perfusion, and end organ damage. Diagnosis of DIC is based on laboratory testing in the right clinical context.13/n" title="So..Fibrin clots in circulationhttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts">trap platelets to make bigger clots https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> micro and macro-vascular thrombosishttps://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Pfeil nach rechts" aria-label="Emoji: Pfeil nach rechts"> ischemia, inadequate perfusion, and end organ damage. Diagnosis of DIC is based on laboratory testing in the right clinical context.13/n" class="img-responsive" style="max-width:100%;"/>


