WHAT IS THE RISK CLASSIFICATION OF THE t(11;14) in MM?
This has been a long-debated question and probably asked in the wrong way. I have always had a special interest in the t(11;14) and want to tell a story and how it relates to venetoclax.
#mmsm #ASH19
1/x
This has been a long-debated question and probably asked in the wrong way. I have always had a special interest in the t(11;14) and want to tell a story and how it relates to venetoclax.
#mmsm #ASH19
1/x
In 1998 we reported the t(11;14) was a poor prognostic marker (only translocation visible in karyotypes). We were seeing the effect of abnormal karyotypes- more growth and tumor burden. @VincentRK
https://onlinelibrary.wiley.com/doi/full/10.1046/j.1365-2141.1998.00700.x?sid=nlm%3Apubmed
https://onlinelibrary.wiley.com/doi/full/... href=" https://www.ncbi.nlm.nih.gov/pubmed/10459351
2/x">https://www.ncbi.nlm.nih.gov/pubmed/10...
https://onlinelibrary.wiley.com/doi/full/10.1046/j.1365-2141.1998.00700.x?sid=nlm%3Apubmed
2/x">https://www.ncbi.nlm.nih.gov/pubmed/10...
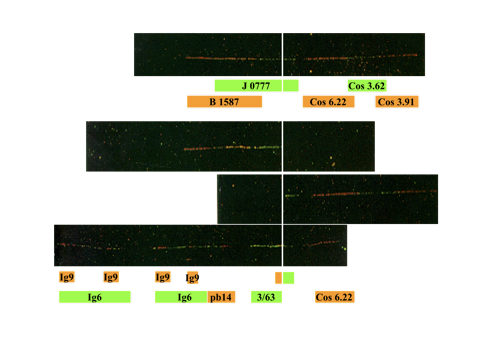
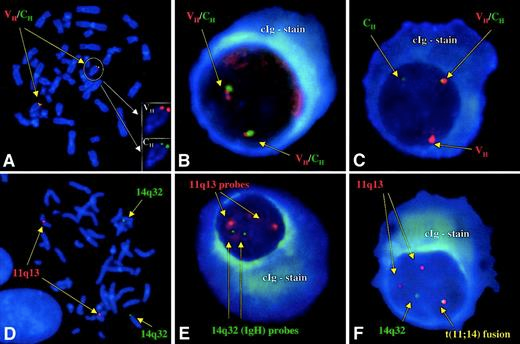
That year I convinced M Gertz to send me to Leiden, Netherlands to study t(11;14) via fiber-FISH- most elegant FISH assay. Only achievable by the great Dutch masters. At my return M Kuehl said “stop wasting your time & start doing interphase FISH.” Best advice!
@MorieGertz
3/x
@MorieGertz
3/x
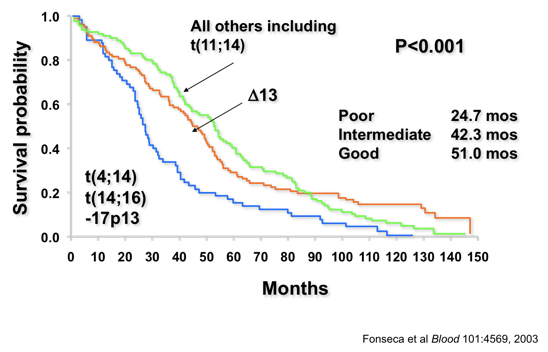
With interphase FISH we reported a prevalence of 15% of MM. It was associated with better outcomes (2003) and subsequently confirmed by others.
KEY POINT: Most of the trials where it was tested had a backbone of alkylators and not any novel agents.
https://www.ncbi.nlm.nih.gov/pubmed/12576322
4/x">https://www.ncbi.nlm.nih.gov/pubmed/12...
KEY POINT: Most of the trials where it was tested had a backbone of alkylators and not any novel agents.
https://www.ncbi.nlm.nih.gov/pubmed/12576322
4/x">https://www.ncbi.nlm.nih.gov/pubmed/12...
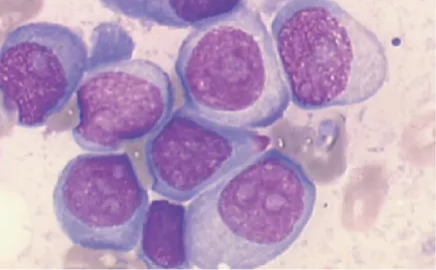
THIS IS AN IMPORTANT POINT: The t(11;14) is known to be associated with lymphoplasmacytic morphology and CD20 expression. Often hyposecretory or (non-secretory) and IgG lambda type.
AGAIN KEY POINT: MM with t(11;14) often has scant cytoplasm (more later).
5/x
AGAIN KEY POINT: MM with t(11;14) often has scant cytoplasm (more later).
5/x
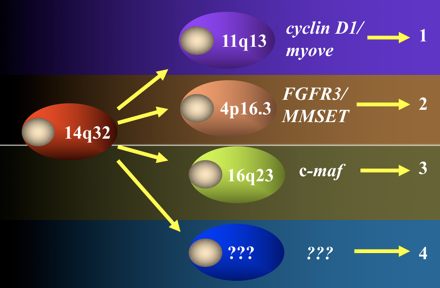
We had this theory called the “Donor Chromosome Theory.” It postulated all MM would have 14q32 translocations. This came after Kuehl, Chesi & Bergsagel had identified translocations as ubiquitous in cell lines & discovered the t(4;14) and t(14;16)
https://www.pnas.org/content/93/24/13931/tab-figures-data
6/x">https://www.pnas.org/content/9...
https://www.pnas.org/content/93/24/13931/tab-figures-data
6/x">https://www.pnas.org/content/9...
In 2001 Dr. Sue Hayman first reported a 50% prevalence in pts with light chain amyloidosis. It was also associated with strong nuclear positivity for cyclin D1. In 2003 H. Avet-Loiseau reported at a high frequency in IgM MM.
https://ashpublications.org/blood/article-lookup/doi/10.1182/blood.v98.7.2266
https://ashpublications.org/blood/art... href=" https://www.ncbi.nlm.nih.gov/pubmed/12393502
7/x">https://www.ncbi.nlm.nih.gov/pubmed/12...
https://ashpublications.org/blood/article-lookup/doi/10.1182/blood.v98.7.2266
7/x">https://www.ncbi.nlm.nih.gov/pubmed/12...
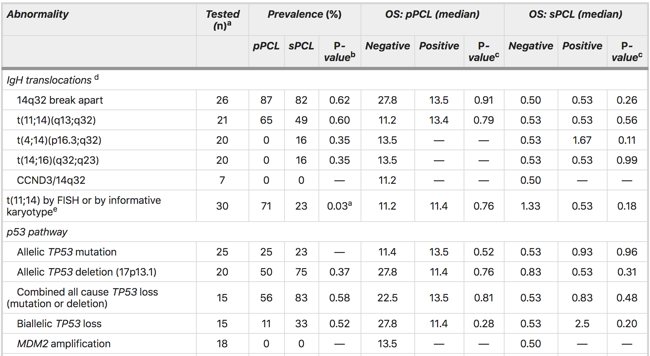
In 2008 we reported the t(11;14) in 50% of cases with primary plasma cell leukemia, not so in sPCL. Others had also reported similar findings. If you “tickle” a MM cell with a t(11;14) it can behave badly!
https://www.ncbi.nlm.nih.gov/pubmed/18216867
8/x">https://www.ncbi.nlm.nih.gov/pubmed/18...
https://www.ncbi.nlm.nih.gov/pubmed/18216867
8/x">https://www.ncbi.nlm.nih.gov/pubmed/18...
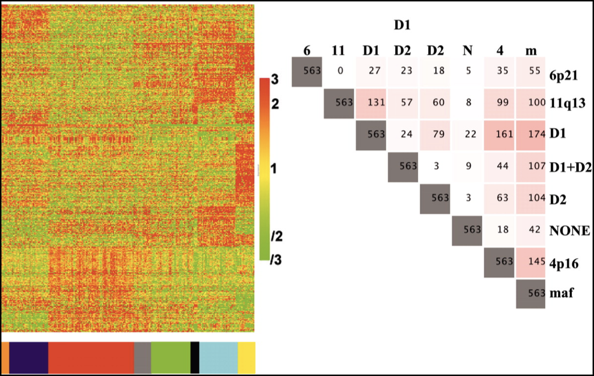
In 2005 Bergsagel and Kuehl proposed the TC classification of MM via gene expression, showed the GEP signature of t(11;14) was identical to that of the t(6;14). Venetoclax? Also, UAMS showed two subtypes of t(11;14): CD1 and CD2. CD1 is better!
https://www.ncbi.nlm.nih.gov/pubmed/16155016
9/x">https://www.ncbi.nlm.nih.gov/pubmed/16...
https://www.ncbi.nlm.nih.gov/pubmed/16155016
9/x">https://www.ncbi.nlm.nih.gov/pubmed/16...
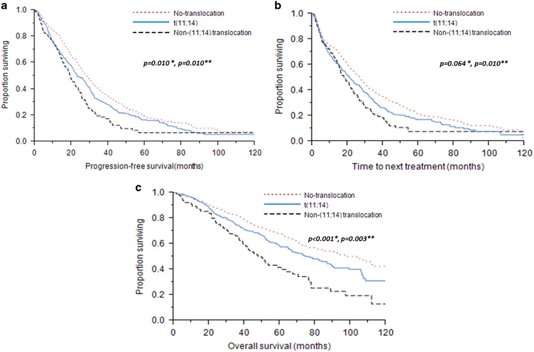
As time went by its prognostic significance seemed to worsen. Could this be related to the Rx used? While all MM outcomes improved it appeared the t(11;14) had stagnated. Lakshman showed inferior ORR, PFS, and OS compared with standard risk pts.
https://www.ncbi.nlm.nih.gov/pubmed/28655925
10/x">https://www.ncbi.nlm.nih.gov/pubmed/28...
https://www.ncbi.nlm.nih.gov/pubmed/28655925
10/x">https://www.ncbi.nlm.nih.gov/pubmed/28...
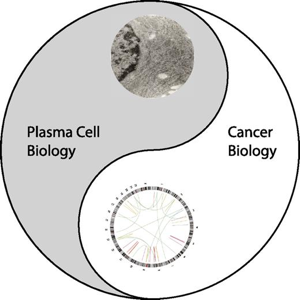
In a seminal observation in 2014 Boise proposed the “Tao of myeloma.” Hypothesis; effective treatments against MM could be built targeting NORMAL PLASMA CELL DIFFERENTIATION, not the genetic changes of the cells, but rather natural vulnerabilities.
https://ashpublications.org/blood/article-lookup/doi/10.1182/blood-2014-05-578732
11/x">https://ashpublications.org/blood/art...
https://ashpublications.org/blood/article-lookup/doi/10.1182/blood-2014-05-578732
11/x">https://ashpublications.org/blood/art...
This explained why drugs like proteasome inhibitors are predominantly useful in the clinic for late B cells – myeloma and Waldenström, and to some extent in other B cells tumors - not much else. Dr. Tiedeman did some elegant studies in this regard.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4118579/
12/x">https://www.ncbi.nlm.nih.gov/pmc/artic...
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4118579/
12/x">https://www.ncbi.nlm.nih.gov/pmc/artic...
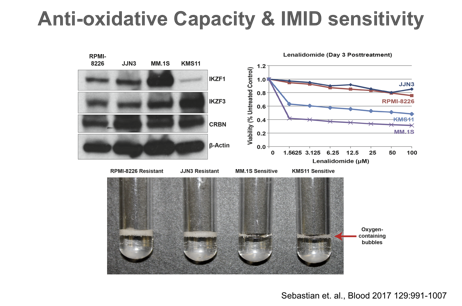
But what about IMIDs? While IMIDS have pleiotropic effects not until recently it was shown that the protein context matters. The group of Florian Basserman showed the chaperon effect of IMIDs & effects on lactate metabolism.
https://www.ncbi.nlm.nih.gov/pubmed/27294876
https://www.ncbi.nlm.nih.gov/pubmed/27... href=" https://ashpublications.org/blood/article/130/Supplement%201/SCI-9/83616
13/x">https://ashpublications.org/blood/art...
https://www.ncbi.nlm.nih.gov/pubmed/27294876
13/x">https://ashpublications.org/blood/art...
During protein folding lots of ROS are produced, and our group showed that IMIDs inhibit detoxifying mechanisms (TrxR). In this case the cells “self-poison.” But to be effective there needs to be abundant protein folding.
https://www.ncbi.nlm.nih.gov/pubmed/27294876
14/x">https://www.ncbi.nlm.nih.gov/pubmed/27...
https://www.ncbi.nlm.nih.gov/pubmed/27294876
14/x">https://www.ncbi.nlm.nih.gov/pubmed/27...
Again IMIDs primarily work in MM, WM, some lymphomas and the only other disease is the 5q- MDS. Again the protein context is essential. Remember MM with t(11;14) is lymphoplasmacytic with scant cytoplasm.
https://www.nature.com/articles/2403091
15/x">https://www.nature.com/articles/...
https://www.nature.com/articles/2403091
15/x">https://www.nature.com/articles/...
How is this related to the t(11;14)? If the cells have less cytoplasm, due to less proteins = less ER stress potential, and thus lower effect of PIs and IMIDs. Thus these drugs work better in “plump” mature plasma cells like in hyperdiploid MM, rather than in t(11;14).
16/x
16/x
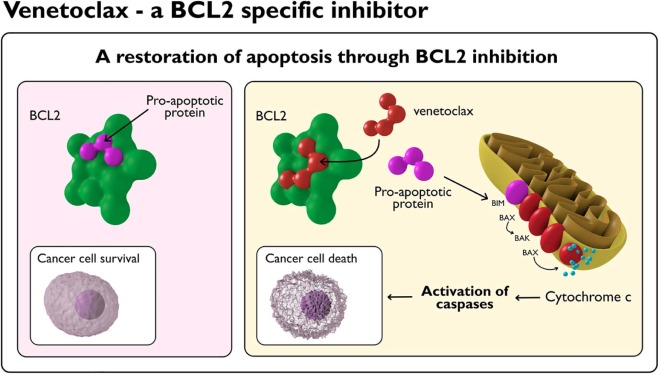
And then came venetoclax! Investigators showed that venetoclax showed great promise in MM with the t(11;14) as this genetic subset depends more on anti-apoptotic signaling (pro-survival to avoid the double negative) of bcl-2.
https://www.ncbi.nlm.nih.gov/pubmed/29018077
17/x">https://www.ncbi.nlm.nih.gov/pubmed/29...
https://www.ncbi.nlm.nih.gov/pubmed/29018077
17/x">https://www.ncbi.nlm.nih.gov/pubmed/29...
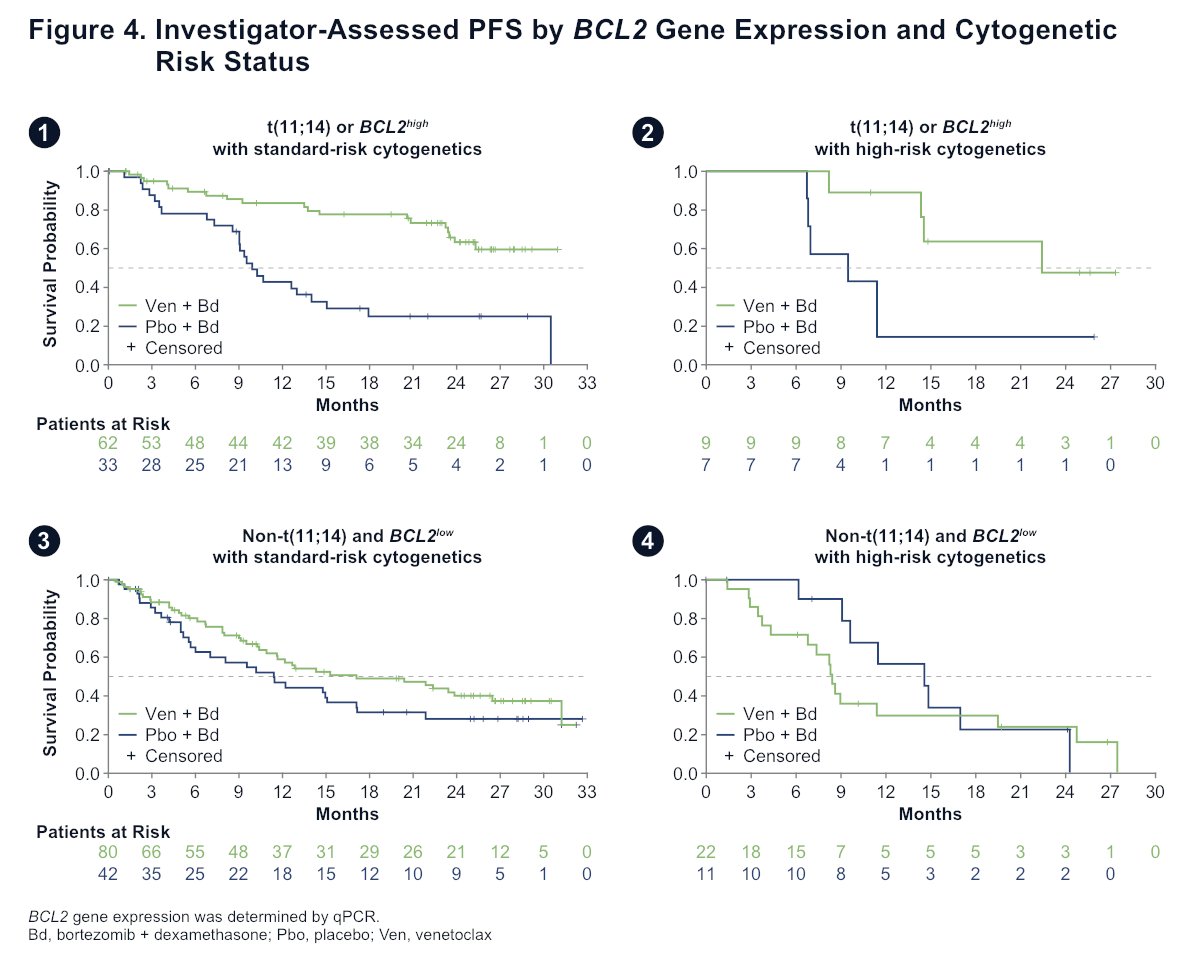
Again, the work of Drs. Boise, Bahlis and Neri has shown that both t(11;14), and perhaps also elevated level of expression of bcl-2 predict a better response to venetoclax. This is truly the first targeted Rx for a specific genetic subset of MM.
https://twitter.com/Rfonsi1/status/1204181561219977216?s=20
18/x">https://twitter.com/Rfonsi1/s...
https://twitter.com/Rfonsi1/status/1204181561219977216?s=20
18/x">https://twitter.com/Rfonsi1/s...
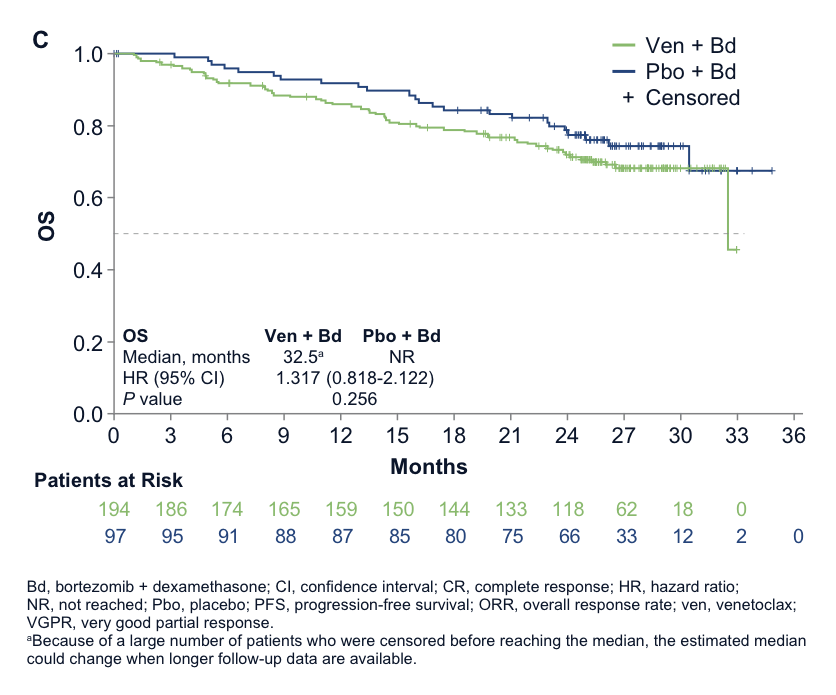
So what happened with the BELLINI trial? In hindsight this trial had a major flaw- venetoclax was tested without selection for t(11;14). Given increased mortality, the trial was stopped, and the FDA paused venetoclax development.
https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-risks-associated-investigational-use-venclexta-multiple-myeloma
19/x">https://www.fda.gov/drugs/dru...
https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-risks-associated-investigational-use-venclexta-multiple-myeloma
19/x">https://www.fda.gov/drugs/dru...
Subsequent analyses have shown that venetoclax is indeed of great benefit for patients with t(11;14), presented at EHA and ASH by Dr. Shaji Kumar and Moreau.
https://twitter.com/Rfonsi1/status/1201233578987642880?s=20
20/x">https://twitter.com/Rfonsi1/s...
https://twitter.com/Rfonsi1/status/1201233578987642880?s=20
20/x">https://twitter.com/Rfonsi1/s...
So the theory of the Tao of myeloma holds and we have now a targeted therapy for MM with t(11;14). If you do not have enough proteins the PI/IMID combination will work, but “not as well.” We urgently need FDA approval for this indication.
21/x
21/x
So what follows?
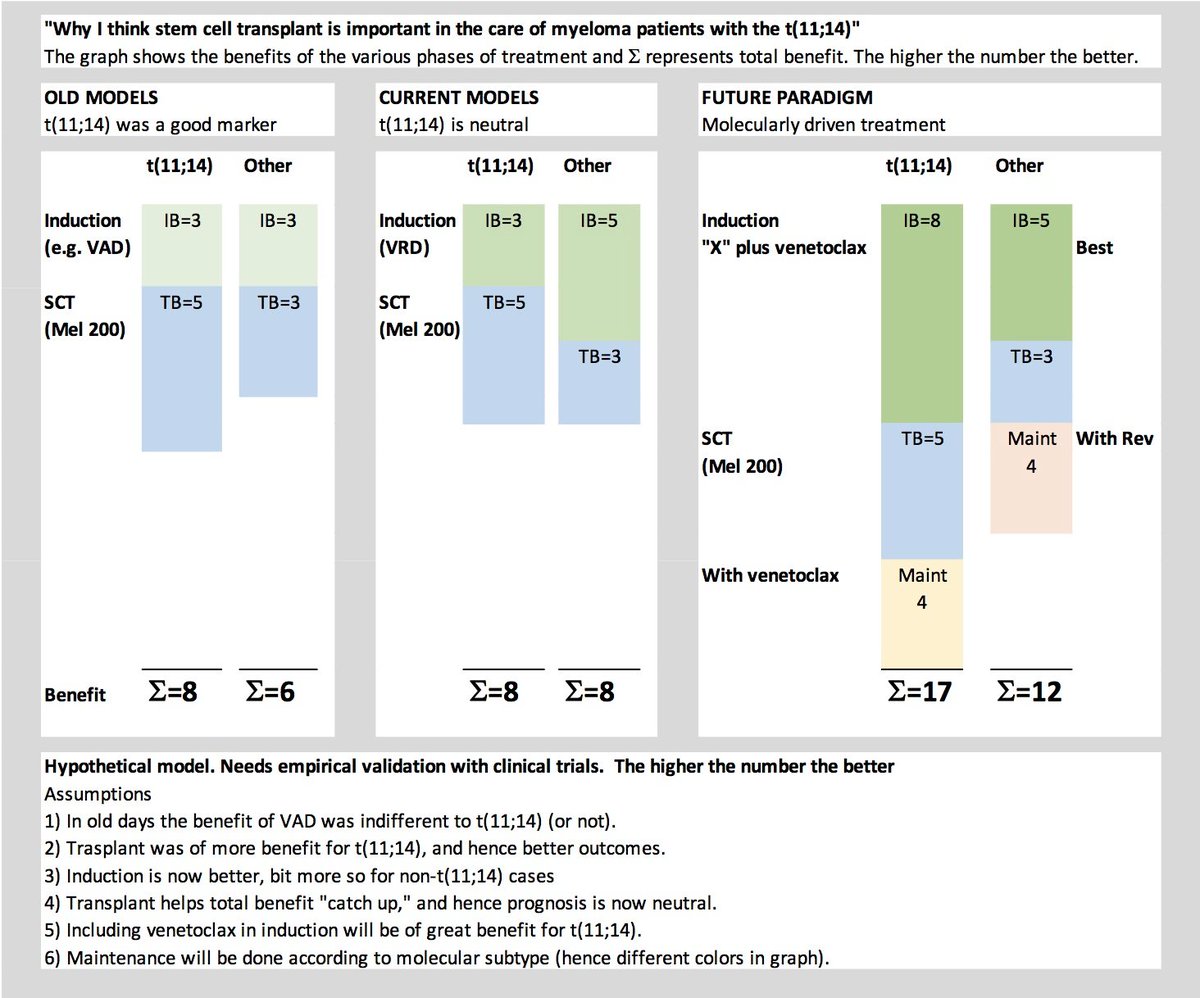
First, IMHO SCT should not be delayed in pts with t(11;14). The benefit was presented at ASH. Another study conducted by the IMWG suggests patients can do well if properly treated.
https://twitter.com/Rfonsi1/status/1205866168214409219?s=20
https://twitter.com/Rfonsi1/s... href=" https://twitter.com/Rfonsi1/status/1205901541036609536?s=20
22/x">https://twitter.com/Rfonsi1/s...
First, IMHO SCT should not be delayed in pts with t(11;14). The benefit was presented at ASH. Another study conducted by the IMWG suggests patients can do well if properly treated.
https://twitter.com/Rfonsi1/status/1205866168214409219?s=20
22/x">https://twitter.com/Rfonsi1/s...
How about Rx of AL? Indeed, in AL the presence of this translocation is a negative prognostic marker for CyBORD treatment. In AL it is particularly important to achieve very deep responses (CR, nFLC). So clinical trials are urgently needed and ongoing for venetoclax in AL.
23/x
23/x
The same is true in pPCL. In patients with t(11;14) the addition of venetoclax is being tested in trials. Again another instance where very deep responses are needed.
24/x
24/x
In the setting of RR MM venetoclax is being tested in combinations. L Boise tells me that at a minimum it always should be started in combination with dexamethasone, but I think more is needed. Trials testing combos with bortezomib, carfilzomib and daratumumab are ongoing.
25/x
25/x
What about SMM with t(11;14). I submit to you (not a recommendation for now) that it will be better to treat SMM with t(11;14) with venetoclax (combinations) than with IMIDs. Trials ongoing.
26/x
26/x
What about maintenance for post SCT t(11;14) patients?
27/x
27/x
So in the end it is not about risk status. It is about a different biology and the correct treatment. Much like having a student who does not do well in school and you only later realize he needs glasses. The end!
28/x
#t1114
28/x
#t1114
ADDENDUM: I have been asked to try to explain why I think stem cell transplant is particularly important for t(11;14). This is a conceptual slide that shows my hypothesis and thinking in this regard.
#mmsm
#mmsm

 Read on Twitter
Read on Twitter https://www.ncbi.nlm.nih.gov/pubmed/10..." title="In 1998 we reported the t(11;14) was a poor prognostic marker (only translocation visible in karyotypes). We were seeing the effect of abnormal karyotypes- more growth and tumor burden. @VincentRK https://onlinelibrary.wiley.com/doi/full/... href=" https://www.ncbi.nlm.nih.gov/pubmed/10459351 2/x">https://www.ncbi.nlm.nih.gov/pubmed/10..." class="img-responsive" style="max-width:100%;"/>
https://www.ncbi.nlm.nih.gov/pubmed/10..." title="In 1998 we reported the t(11;14) was a poor prognostic marker (only translocation visible in karyotypes). We were seeing the effect of abnormal karyotypes- more growth and tumor burden. @VincentRK https://onlinelibrary.wiley.com/doi/full/... href=" https://www.ncbi.nlm.nih.gov/pubmed/10459351 2/x">https://www.ncbi.nlm.nih.gov/pubmed/10..." class="img-responsive" style="max-width:100%;"/>
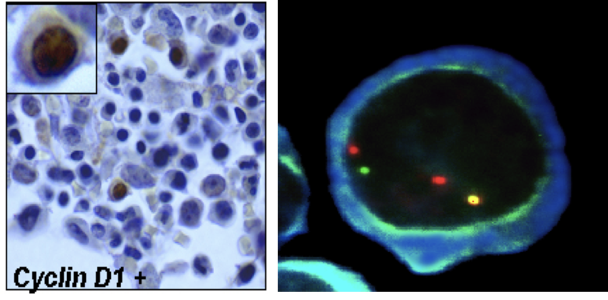
 https://www.ncbi.nlm.nih.gov/pubmed/12..." title="In 2001 Dr. Sue Hayman first reported a 50% prevalence in pts with light chain amyloidosis. It was also associated with strong nuclear positivity for cyclin D1. In 2003 H. Avet-Loiseau reported at a high frequency in IgM MM. https://ashpublications.org/blood/art... href=" https://www.ncbi.nlm.nih.gov/pubmed/12393502 7/x">https://www.ncbi.nlm.nih.gov/pubmed/12..." class="img-responsive" style="max-width:100%;"/>
https://www.ncbi.nlm.nih.gov/pubmed/12..." title="In 2001 Dr. Sue Hayman first reported a 50% prevalence in pts with light chain amyloidosis. It was also associated with strong nuclear positivity for cyclin D1. In 2003 H. Avet-Loiseau reported at a high frequency in IgM MM. https://ashpublications.org/blood/art... href=" https://www.ncbi.nlm.nih.gov/pubmed/12393502 7/x">https://www.ncbi.nlm.nih.gov/pubmed/12..." class="img-responsive" style="max-width:100%;"/>