Part 1 of 2 | MCQ in 2nd Part 2:
23M active IV heroin user p/w 4 d fever/headache/seizure. Temp 39.3, supple neck. Initial head CT (-). CSF: WBC 30 (60% L), TP 90, gluc n/l. Developed R arm/leg hemiparesis hospital day 5. MRI: large L>R b/l basal ganglia enhancing lesions ( https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index">)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index">)
23M active IV heroin user p/w 4 d fever/headache/seizure. Temp 39.3, supple neck. Initial head CT (-). CSF: WBC 30 (60% L), TP 90, gluc n/l. Developed R arm/leg hemiparesis hospital day 5. MRI: large L>R b/l basal ganglia enhancing lesions (
|Part 2 of 2 |
Routine CSF viral PCRs/bacterial/AFB/fungal Cxs (-). Blood Cxs, HIV, RPR, TEE (-). Lives in Missouri, no travel/other exposures. Continued to be highly febrile on cefepime/vancomycin/metronidazole. What is the most likely cause of his clinical presentation?
Routine CSF viral PCRs/bacterial/AFB/fungal Cxs (-). Blood Cxs, HIV, RPR, TEE (-). Lives in Missouri, no travel/other exposures. Continued to be highly febrile on cefepime/vancomycin/metronidazole. What is the most likely cause of his clinical presentation?
1/9
Only 37% got the correct answer, Mucor.
Learning points:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> High risk of cerebral mucormycosis among people who inject drugs (PWID)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> High risk of cerebral mucormycosis among people who inject drugs (PWID)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Unique basal ganglia involvement seen in these cases
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Unique basal ganglia involvement seen in these cases
Picture in MCQ taken from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3590060/">https://www.ncbi.nlm.nih.gov/pmc/artic...
Only 37% got the correct answer, Mucor.
Learning points:
Picture in MCQ taken from:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3590060/">https://www.ncbi.nlm.nih.gov/pmc/artic...
2/9
We& #39;ve recently discussed some of the infections seen among PWID https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> https://twitter.com/WuidQ/status/1191477822579204104?s=20
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index"> https://twitter.com/WuidQ/status/1191477822579204104?s=20
Isolated">https://twitter.com/WuidQ/sta... cerebral mucromycosis is one these infections clinicians need to be aware of. \
This MCQ was inspired by a case presented in our #idgrandrounds in 2015.
We& #39;ve recently discussed some of the infections seen among PWID
Isolated">https://twitter.com/WuidQ/sta... cerebral mucromycosis is one these infections clinicians need to be aware of. \
This MCQ was inspired by a case presented in our #idgrandrounds in 2015.
3/9
Common Mucor risk factors:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> DM in DKA, steroids, hematologic malignancies, transplantation, neutropenia, trauma/burns
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> DM in DKA, steroids, hematologic malignancies, transplantation, neutropenia, trauma/burns
Common forms:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Rhino-orbito-cerebral | pulmonary | disseminated > GI
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Rhino-orbito-cerebral | pulmonary | disseminated > GI
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Cutaneous (trauma/burn)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Cutaneous (trauma/burn)
Isolated Mucor:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Renal & cerebral seen in PWID
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Renal & cerebral seen in PWID
Common Mucor risk factors:
Common forms:
Isolated Mucor:
4/9
Isolated cerebral Mucor in PWID:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one"> Predilection for the basal ganglia (uni-/bi lateral)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="1⃣" title="Keycap digit one" aria-label="Emoji: Keycap digit one"> Predilection for the basal ganglia (uni-/bi lateral)
Case series: 20 of 22 patients have basal ganglia involvement
https://www.ncbi.nlm.nih.gov/pubmed/7888545
68">https://www.ncbi.nlm.nih.gov/pubmed/78... patients w/ isolated cerebral Mucro https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> 82% PWID, 71%
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> 82% PWID, 71%  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign">basal ganglia
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign">basal ganglia
https://www.ncbi.nlm.nih.gov/pubmed/30415043 ">https://www.ncbi.nlm.nih.gov/pubmed/30...
Isolated cerebral Mucor in PWID:
Case series: 20 of 22 patients have basal ganglia involvement
https://www.ncbi.nlm.nih.gov/pubmed/7888545
68">https://www.ncbi.nlm.nih.gov/pubmed/78... patients w/ isolated cerebral Mucro
https://www.ncbi.nlm.nih.gov/pubmed/30415043 ">https://www.ncbi.nlm.nih.gov/pubmed/30...
5/9
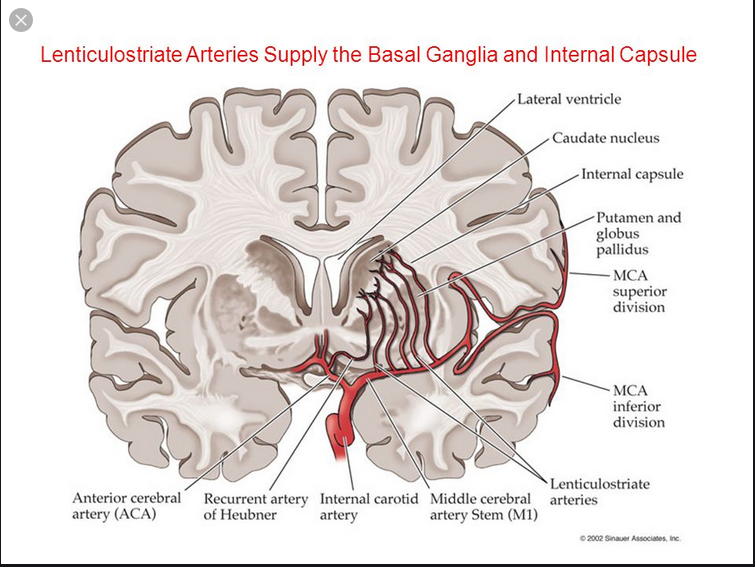
Why the basal ganglia?
Mucor, highly angioinvasive. Tissue infarction/necrosis, path hallmarks.
https://academic.oup.com/cid/article/45/11/1522/335289
Contaminated">https://academic.oup.com/cid/artic... injection https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign"> microvascular injury from injected drug
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign"> microvascular injury from injected drug  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> seeding to highly vascularized area (small penetrating arterioles/collaterals)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> seeding to highly vascularized area (small penetrating arterioles/collaterals)
Why the basal ganglia?
Mucor, highly angioinvasive. Tissue infarction/necrosis, path hallmarks.
https://academic.oup.com/cid/article/45/11/1522/335289
Contaminated">https://academic.oup.com/cid/artic... injection
6/9
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two"> Need to have a high index of suspicion (can lead to early dx & tx)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="2⃣" title="Keycap digit two" aria-label="Emoji: Keycap digit two"> Need to have a high index of suspicion (can lead to early dx & tx)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Can present like typical meningitis (fever, mental status change, headache); but almost 50%,
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Can present like typical meningitis (fever, mental status change, headache); but almost 50%, https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign">hemiparesis
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign">hemiparesis
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Rapidly progressive course despite abx
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Rapidly progressive course despite abx
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Brain biopsy is diagnostic (only 38% had
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Brain biopsy is diagnostic (only 38% had  https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign">culture)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign">culture)
7/9
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="3⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three"> High mortality rate
https://abs.twimg.com/emoji/v2/... draggable="false" alt="3⃣" title="Keycap digit three" aria-label="Emoji: Keycap digit three"> High mortality rate
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> 65% mortality rate, survival a/w receipt of amphotericin & stereotactic aspiration https://www.ncbi.nlm.nih.gov/pubmed/30415043
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> 65% mortality rate, survival a/w receipt of amphotericin & stereotactic aspiration https://www.ncbi.nlm.nih.gov/pubmed/30415043
Among">https://www.ncbi.nlm.nih.gov/pubmed/30... 70 patients: delay in antifungals (>6 days after dx) led to a 2-fold mortality increase https://academic.oup.com/cid/article/47/4/503/303246">https://academic.oup.com/cid/artic...
Among">https://www.ncbi.nlm.nih.gov/pubmed/30... 70 patients: delay in antifungals (>6 days after dx) led to a 2-fold mortality increase https://academic.oup.com/cid/article/47/4/503/303246">https://academic.oup.com/cid/artic...
8/9
Other answers:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> CNS Toxo is highly unusual in people w/o HIV/immunosuppression
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> CNS Toxo is highly unusual in people w/o HIV/immunosuppression
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Although VZV PCR can miss intracranial VZV vasculopathy, most lesions are in gray-white matter junction
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Although VZV PCR can miss intracranial VZV vasculopathy, most lesions are in gray-white matter junction
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Case lacks findings c/w rabies: hydrophobia, aerophobia, exposure, etc
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Case lacks findings c/w rabies: hydrophobia, aerophobia, exposure, etc
Other answers:
9/9
In summary:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Need to be aware of isolated cerebral Mucor among PWID (high index of suspicion, rapid course, stroke-like presentation, basal ganglia lesions)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Need to be aware of isolated cerebral Mucor among PWID (high index of suspicion, rapid course, stroke-like presentation, basal ganglia lesions)
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Early suspicion, early Tx and Dx
https://abs.twimg.com/emoji/v2/... draggable="false" alt="▪️" title="Black small square" aria-label="Emoji: Black small square"> Early suspicion, early Tx and Dx  https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> life saving!
https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> life saving!
In summary:
9/9 EXTRA
In patients w/ cerebral Mucor (like in this featured case), would you use high dose ampho (10 mg/kg/day)?
https://academic.oup.com/jac/article/70/11/3116/2364014
https://academic.oup.com/jac/artic... href="https://twitter.com/FungalDoc">@FungalDoc @GermHunterMD @ShohamTxID @CarlosdelRio7 @PaulSaxMD @RazonableMD @DocWoc71 @BradCutrellMD @Cortes_Penfield
In patients w/ cerebral Mucor (like in this featured case), would you use high dose ampho (10 mg/kg/day)?
https://academic.oup.com/jac/article/70/11/3116/2364014
Thank you for your response @FungalDoc @BradSpellberg @TxID_Edu @jdcooperid @FarhanFazal10.
I remember, this patient unfortunately expired despite higher dose ampho. By the time brain biopsy done & showed molds, might have been too late already.
I remember, this patient unfortunately expired despite higher dose ampho. By the time brain biopsy done & showed molds, might have been too late already.

 Read on Twitter
Read on Twitter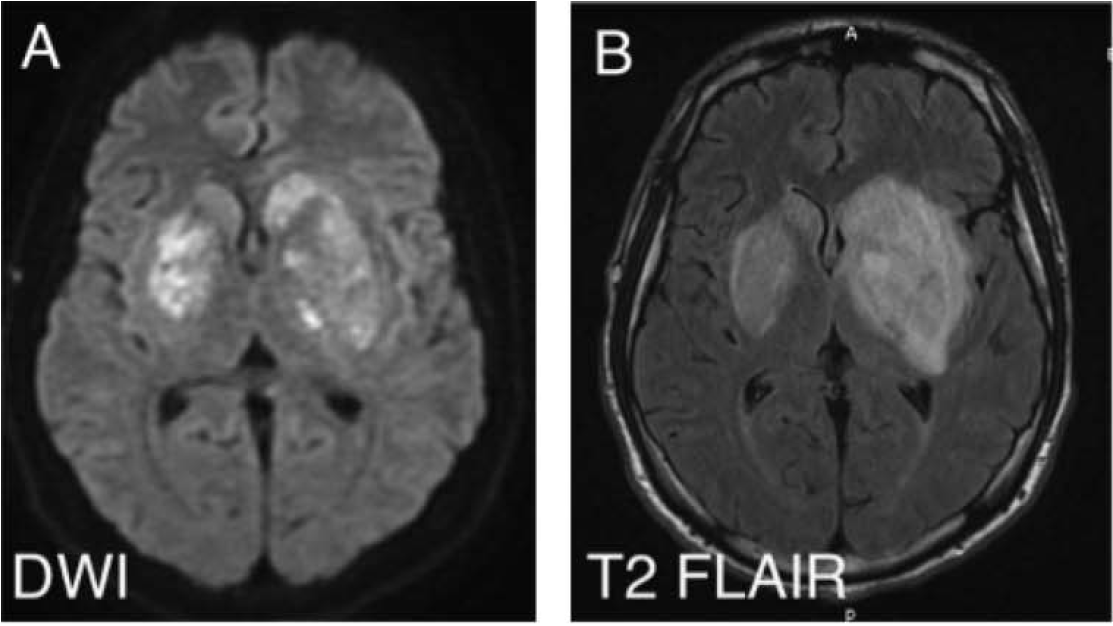 )" title="Part 1 of 2 | MCQ in 2nd Part 2:23M active IV heroin user p/w 4 d fever/headache/seizure. Temp 39.3, supple neck. Initial head CT (-). CSF: WBC 30 (60% L), TP 90, gluc n/l. Developed R arm/leg hemiparesis hospital day 5. MRI: large L>R b/l basal ganglia enhancing lesions (https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index">)" class="img-responsive" style="max-width:100%;"/>
)" title="Part 1 of 2 | MCQ in 2nd Part 2:23M active IV heroin user p/w 4 d fever/headache/seizure. Temp 39.3, supple neck. Initial head CT (-). CSF: WBC 30 (60% L), TP 90, gluc n/l. Developed R arm/leg hemiparesis hospital day 5. MRI: large L>R b/l basal ganglia enhancing lesions (https://abs.twimg.com/emoji/v2/... draggable="false" alt="👇" title="Down pointing backhand index" aria-label="Emoji: Down pointing backhand index">)" class="img-responsive" style="max-width:100%;"/>
 High risk of cerebral mucormycosis among people who inject drugs (PWID)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Unique basal ganglia involvement seen in these casesPicture in MCQ taken from: https://www.ncbi.nlm.nih.gov/pmc/artic..." title="1/9Only 37% got the correct answer, Mucor.Learning points:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> High risk of cerebral mucormycosis among people who inject drugs (PWID)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Unique basal ganglia involvement seen in these casesPicture in MCQ taken from: https://www.ncbi.nlm.nih.gov/pmc/artic..." class="img-responsive" style="max-width:100%;"/>
High risk of cerebral mucormycosis among people who inject drugs (PWID)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Unique basal ganglia involvement seen in these casesPicture in MCQ taken from: https://www.ncbi.nlm.nih.gov/pmc/artic..." title="1/9Only 37% got the correct answer, Mucor.Learning points:https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> High risk of cerebral mucormycosis among people who inject drugs (PWID)https://abs.twimg.com/emoji/v2/... draggable="false" alt="✔️" title="Heavy check mark" aria-label="Emoji: Heavy check mark"> Unique basal ganglia involvement seen in these casesPicture in MCQ taken from: https://www.ncbi.nlm.nih.gov/pmc/artic..." class="img-responsive" style="max-width:100%;"/>
 microvascular injury from injected drug https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> seeding to highly vascularized area (small penetrating arterioles/collaterals)" title="5/9Why the basal ganglia? Mucor, highly angioinvasive. Tissue infarction/necrosis, path hallmarks. https://academic.oup.com/cid/artic... injection https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign"> microvascular injury from injected drug https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> seeding to highly vascularized area (small penetrating arterioles/collaterals)" class="img-responsive" style="max-width:100%;"/>
microvascular injury from injected drug https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> seeding to highly vascularized area (small penetrating arterioles/collaterals)" title="5/9Why the basal ganglia? Mucor, highly angioinvasive. Tissue infarction/necrosis, path hallmarks. https://academic.oup.com/cid/artic... injection https://abs.twimg.com/emoji/v2/... draggable="false" alt="➕" title="Heavy plus sign" aria-label="Emoji: Heavy plus sign"> microvascular injury from injected drug https://abs.twimg.com/emoji/v2/... draggable="false" alt="👉" title="Right pointing backhand index" aria-label="Emoji: Right pointing backhand index"> seeding to highly vascularized area (small penetrating arterioles/collaterals)" class="img-responsive" style="max-width:100%;"/>


