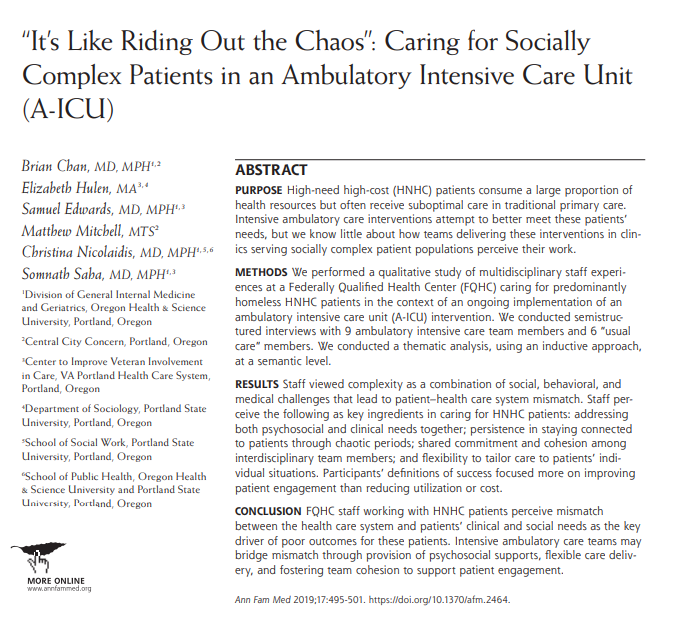
How do multi-disc staff caring for medically and socially complex patients in an Ambulatory "ICU" care model view their work?
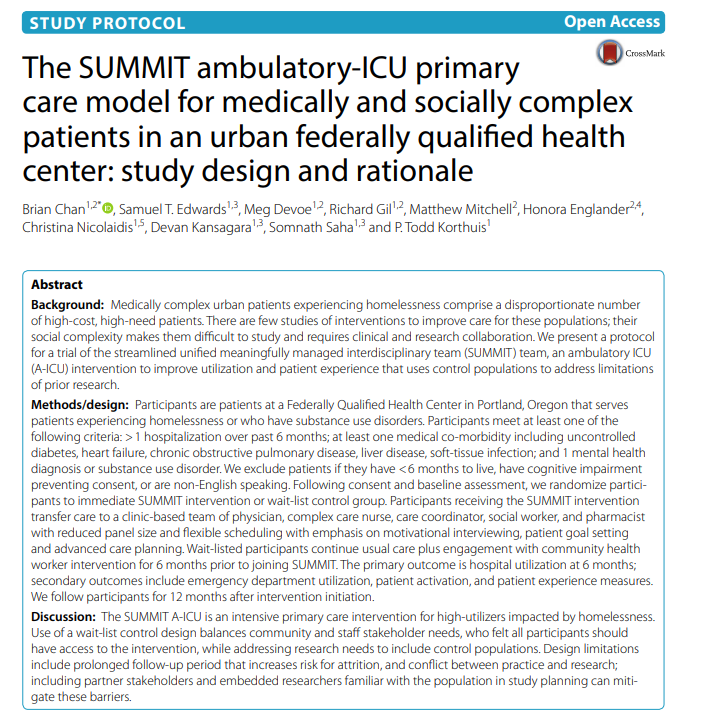
Presenting our teams qualitative work evaluating SUMMIT A-ICU at an urban FQHC with high rates homelessness, SUDs
http://www.annfammed.org/content/17/6/495">https://www.annfammed.org/content/1...
Presenting our teams qualitative work evaluating SUMMIT A-ICU at an urban FQHC with high rates homelessness, SUDs
http://www.annfammed.org/content/17/6/495">https://www.annfammed.org/content/1...
Our question was how do these A-ICU teams (intensive stand-alone teams with low patient-staff ratios, multi-d staff) work?
See our prior paper on team structure and motivation https://ascpjournal.biomedcentral.com/articles/10.1186/s13722-018-0128-y">https://ascpjournal.biomedcentral.com/articles/...
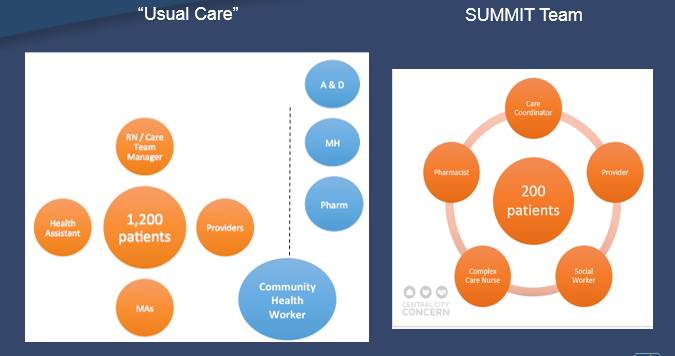
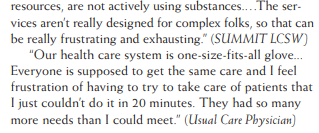
We identified 7 themes: 1) multiple dimensions of complexity (not just medical); 2) team members feel they are addressing patient-system mismatches ..
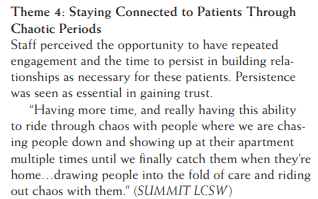
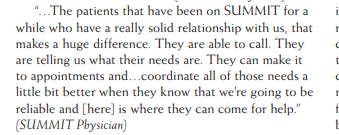
A-ICU staff felt they added value by: 3) addressing both medical and psychosocial need; 4) sitting with patients during chaotic times; 5) fostering team cohesion and shared commitment to patients; 6) ability to deliver flexible care
final theme (7) was defining "success" - not nec by utilization decreases but by increased engagement, observing building of trust
Final thoughts: 1) honored to work along side this care team, patients, and researchers; 2) can we scale this up beyond our urban FQHC; 3) doesn& #39;t this sound like how primary care should/could be for all patients, providers, systems? @samedwardsmd @AnnFamMed @gabefabreau

 Read on Twitter
Read on Twitter