Interesting study findings in @JAMA_current article published yesterday:
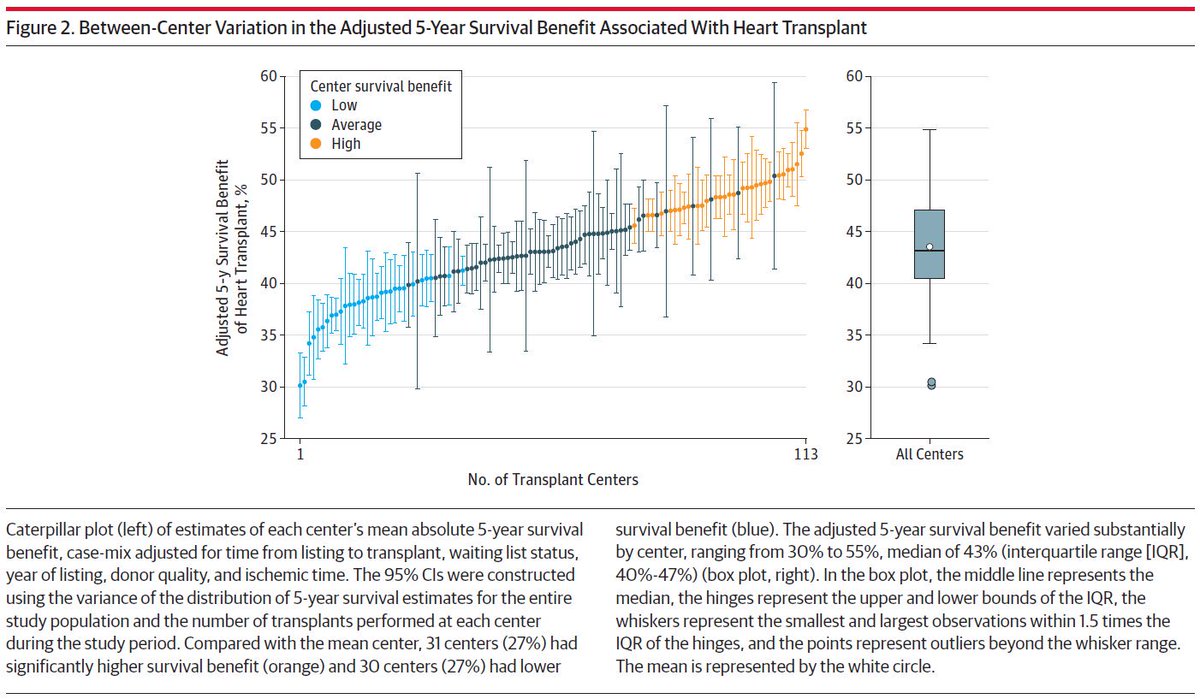
1) The 5-year survival benefit assoc with heart tx varied across centers, and
2) High survival benefit centers performed heart tx for patients with lower estimated waiting list survival without transplant
1) The 5-year survival benefit assoc with heart tx varied across centers, and
2) High survival benefit centers performed heart tx for patients with lower estimated waiting list survival without transplant
Link to article: https://jamanetwork.com/journals/jama/fullarticle/2754791">https://jamanetwork.com/journals/...
Pretty impressive variation in 5-yr survival benefit across hospitals (although my epi brain is screaming at me for the truncated y-axis, which tends to exaggerate variation).
Figure 3 looks under the hood a bit more to show that the added survival benefit is largely driven by low candidate survival
i.e., centers with the largest survival benefit of heart tx had treated patients with the lowest survival without a heart tx
i.e., centers with the largest survival benefit of heart tx had treated patients with the lowest survival without a heart tx
Note that in the second pane, there was little correlation between post-tx survival and overall survival benefit.
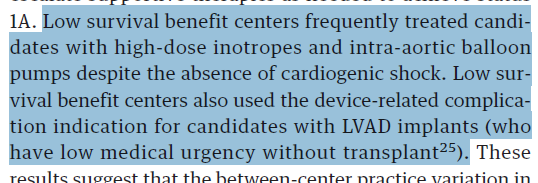
The new allocation system may mitigate some variability by reserving heart tx for the sickest pts:
"If one applies the new cardiogenic shock criteria conservatively in the 6-tier allocation system, one-third of status 1A recipients would not qualify for
status 1, 2, or 3."
"If one applies the new cardiogenic shock criteria conservatively in the 6-tier allocation system, one-third of status 1A recipients would not qualify for
status 1, 2, or 3."
The cynical side of me thinks that changing the rules will just create new incentives to play to the test, such as big upcoding in cardiogenic shock, or even more worrying, greater/more inappropriate use of ECMO, mechanical circ support, or ventilation.
Seems like a ripe area for research down the road, particularly around the potential adverse effects of the new tier allocation system.
cc @boback @mad_sters @iamritu @bnallamo @TomCascinoMD
cc @boback @mad_sters @iamritu @bnallamo @TomCascinoMD

 Read on Twitter
Read on Twitter