THREAD: I& #39;m often asked whether the #SDoH & upstream inequities impact people later in life, when they are in need of #palliativecare & end-of-life care. A newly updated @HQOntario report paints a vivid picture.
#cdnhealth #onhealth #hpm #medtwitter
https://www.hqontario.ca/System-Performance/Specialized-Reports/Palliative-Care-Report">https://www.hqontario.ca/System-Pe...
#cdnhealth #onhealth #hpm #medtwitter
https://www.hqontario.ca/System-Performance/Specialized-Reports/Palliative-Care-Report">https://www.hqontario.ca/System-Pe...
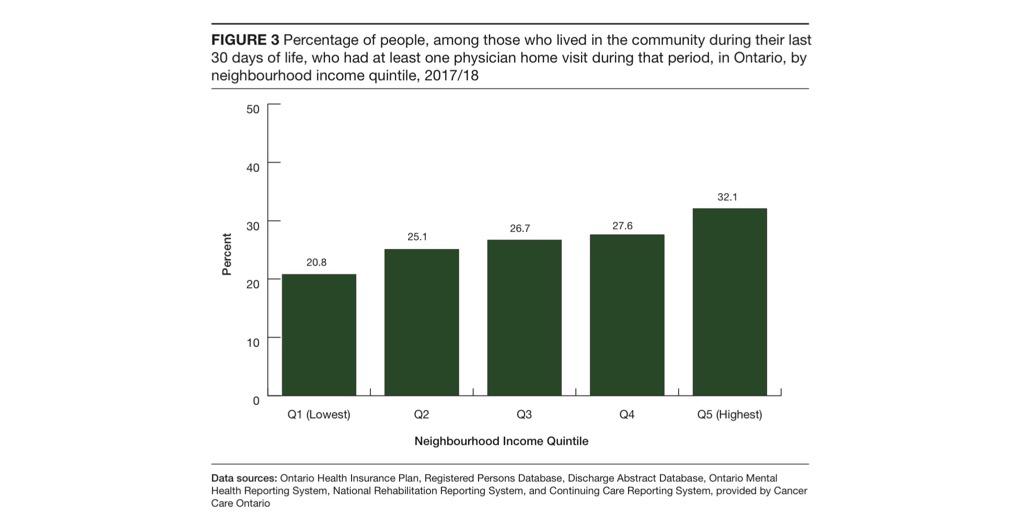
1. Regardless of how sick you may be in #Ontario, your income status (a vital #SDoH), majorly influences whether or not you receive #PalliativeCare, if at all.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below
2. People near the end-of-life who are living in higher-income neighbourhoods are more likely to receive a home visit from a doctor during their final 30 days of life.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> 32.1% in wealthiest vs 20.8% in poorest neighbourhoods
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> 32.1% in wealthiest vs 20.8% in poorest neighbourhoods
3. People living in higher-income neighbourhoods are also
more likely to receive home care to help them remain comfortable & address their needs.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Any home care: 55.8% vs 47.2% in poorest neighbourhoods
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Any home care: 55.8% vs 47.2% in poorest neighbourhoods
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Palliative-specific: 29.2% vs 21.2% in poorest neighbourhoods
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Palliative-specific: 29.2% vs 21.2% in poorest neighbourhoods
more likely to receive home care to help them remain comfortable & address their needs.
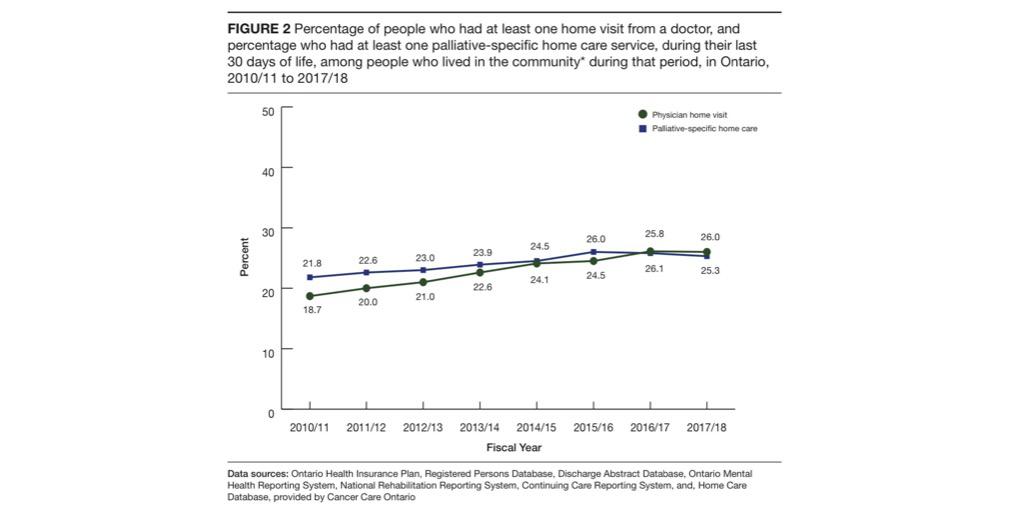
4. Meanwhile, there has been little change over recent years in the proportions of people who receive publicly funded palliative-specific or any home care in their last month of life. Further, rates of home visits in the last month of life has slowed.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below
5. Yet, this data does not reflect those experiencing structural vulnerabilities (eg homelessness, extreme poverty, substance use, trauma, social isolation, mental illness) in need of #palliativecare. So then, how many more are falling through the cracks in our communities?
6. The inequities that stem from the #SDoH surely impact people& #39;s lives, but they also accumulate at the end-of-life.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Death is most certainly a social justice issue.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Death is most certainly a social justice issue.
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Until we start seeing #palliativecare through the lens of #healthequity, little will change.
https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark"> Until we start seeing #palliativecare through the lens of #healthequity, little will change.
/END
/END

 Read on Twitter
Read on Twitter
 See figure below" title="1. Regardless of how sick you may be in #Ontario, your income status (a vital #SDoH), majorly influences whether or not you receive #PalliativeCare, if at all.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below" class="img-responsive" style="max-width:100%;"/>
See figure below" title="1. Regardless of how sick you may be in #Ontario, your income status (a vital #SDoH), majorly influences whether or not you receive #PalliativeCare, if at all.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below" class="img-responsive" style="max-width:100%;"/>
 See figure below" title="4. Meanwhile, there has been little change over recent years in the proportions of people who receive publicly funded palliative-specific or any home care in their last month of life. Further, rates of home visits in the last month of life has slowed.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below" class="img-responsive" style="max-width:100%;"/>
See figure below" title="4. Meanwhile, there has been little change over recent years in the proportions of people who receive publicly funded palliative-specific or any home care in their last month of life. Further, rates of home visits in the last month of life has slowed.https://abs.twimg.com/emoji/v2/... draggable="false" alt="✅" title="White heavy check mark" aria-label="Emoji: White heavy check mark">See figure below" class="img-responsive" style="max-width:100%;"/>


