I promised @rallamee I would stay off Twitter. But "forever" is a long time in science.
John Mandrola, whom I had the honour to lecture with at Roy Coll Phys Edinburgh last week, asked me what I thought of this "complaint letter" he got about his blog article mentioning ORBITA.
John Mandrola, whom I had the honour to lecture with at Roy Coll Phys Edinburgh last week, asked me what I thought of this "complaint letter" he got about his blog article mentioning ORBITA.
In the extract above, what do you think made me choke on the very nice cream cake the Royal College had provided to us?
[don& #39;t worry, I took an extra statin that night]
[don& #39;t worry, I took an extra statin that night]
Well, let& #39;s look at this.
I am thinking this sentence was prepared on their behalf by an ESC spin team. It is conveying to uninitiated people that counting vessels by *shock horror* looking at them, is backward and out-of-date.
It won& #39;t work on sensible cardiologists: they know that that is how vessels are, in reality, counted.
So I am not too angry about it. If they want to waste their time hoodwinking people, let them do it.
Maybe it is sport for them?
So I am not too angry about it. If they want to waste their time hoodwinking people, let them do it.
Maybe it is sport for them?
Correct. Well done for understanding the protocol.
What was the reason for this?
What was the reason for this?
Everyone is right so far.
But now ...
But now ...
Oh! Wait! Oh my, I have been so wrong!
Yes, you see it now, don& #39;t you! It& #39;s so easy to underestimate these guideline bods.
You do it, I do it, we all do it.
You do it, I do it, we all do it.
Yes, for it is He.
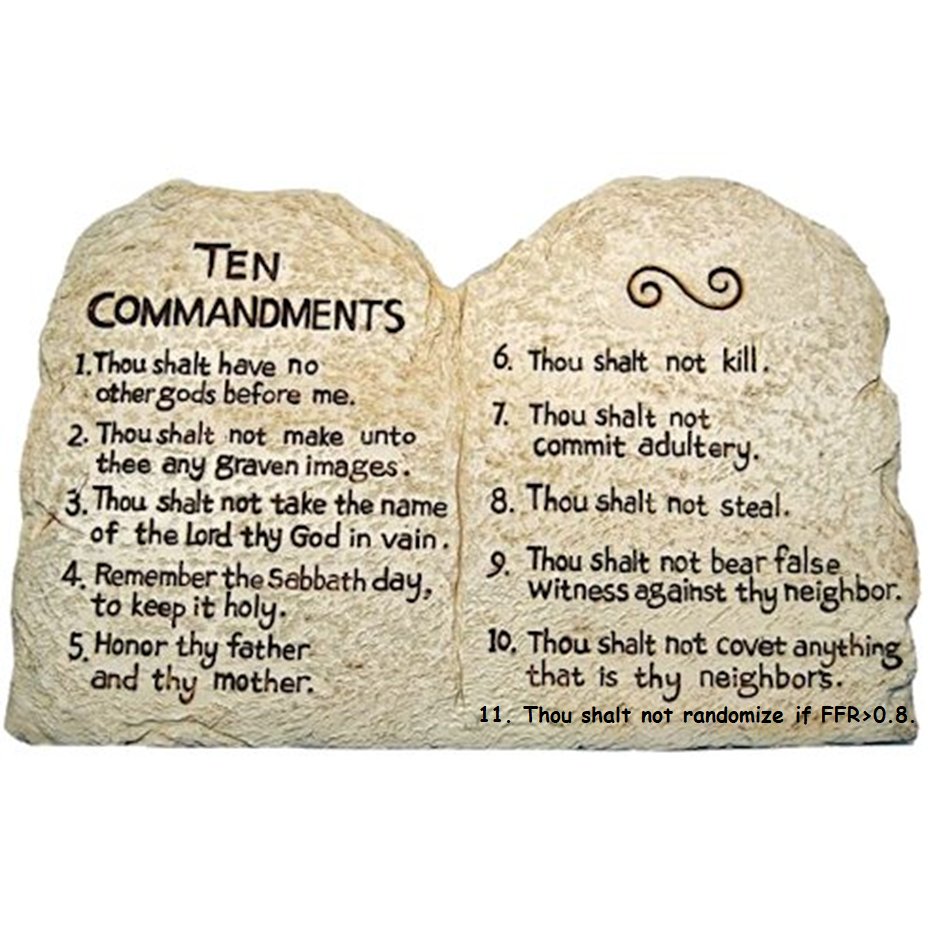
It is indeed Written In Tablets of Stone.
We just hadn& #39;t looked carefully enough before.
I take responsibility for that. I don& #39;t like being careless.
It is indeed Written In Tablets of Stone.
We just hadn& #39;t looked carefully enough before.
I take responsibility for that. I don& #39;t like being careless.
So that explains it then.
Even Top People have higher-ups. After due prayer and meditation, their co-author has informed them that it was a sin to randomize patients who had angina, a tight lesion and a positive ischaemia test.
Even Top People have higher-ups. After due prayer and meditation, their co-author has informed them that it was a sin to randomize patients who had angina, a tight lesion and a positive ischaemia test.
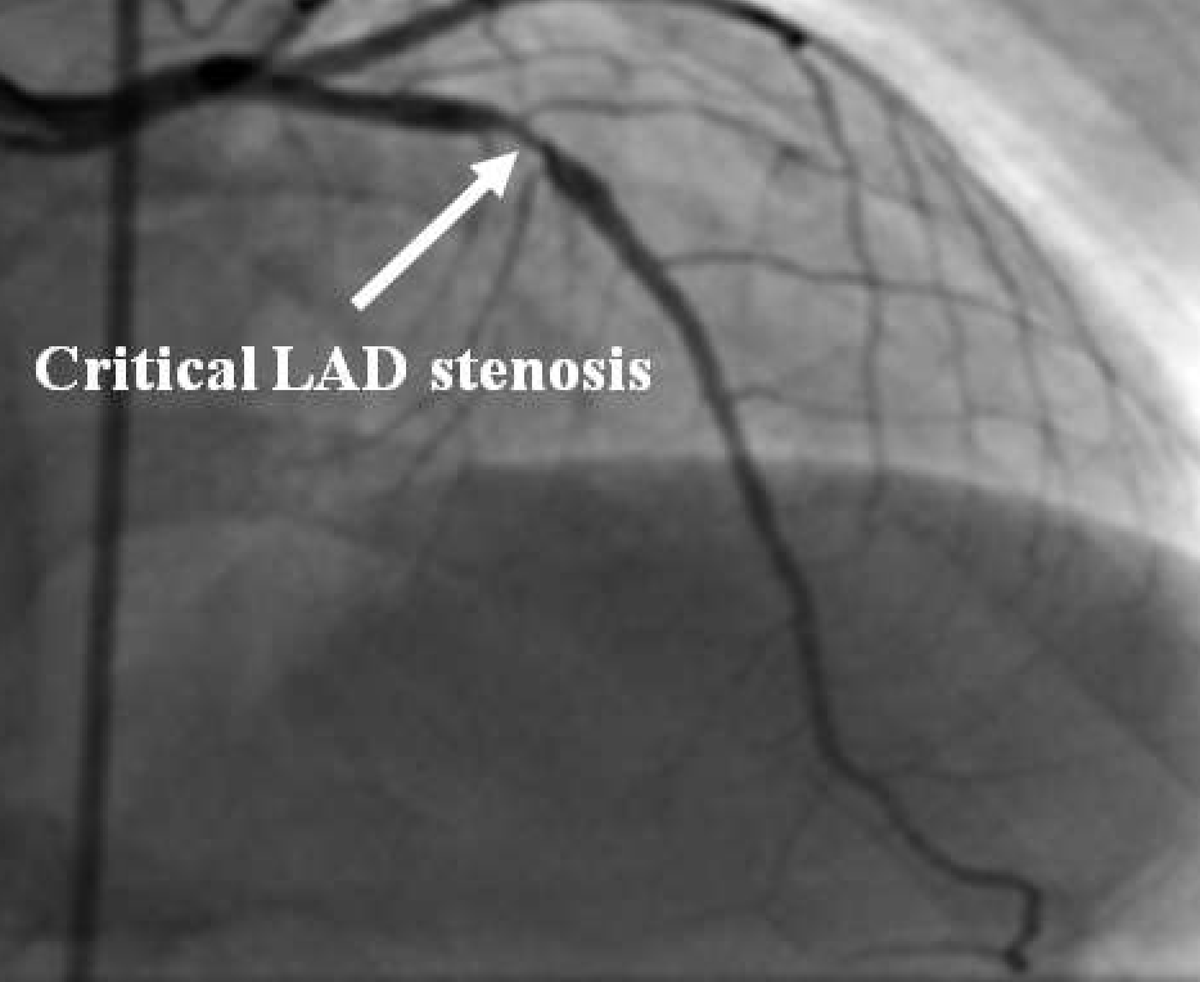
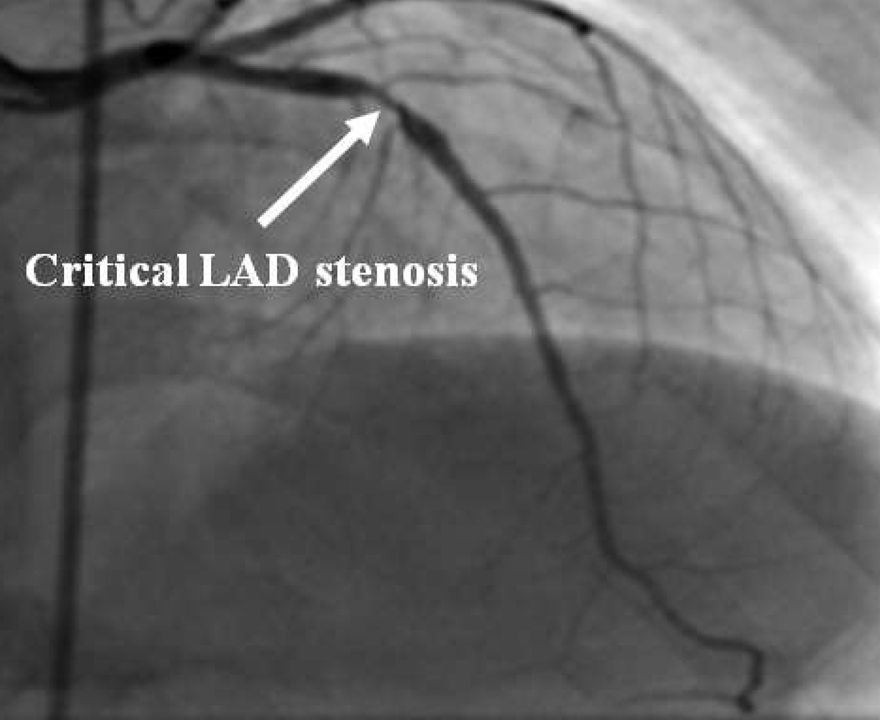
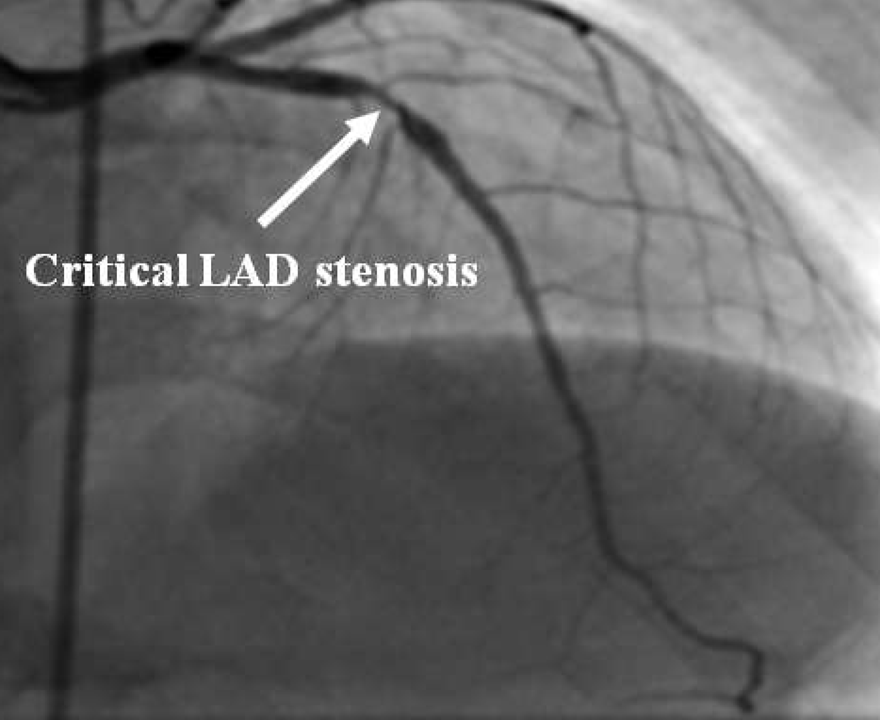
Stress Echo is positive for inducible ischaemia.
By the way, for the previous scenario (let& #39;s call it "A"), I agree with both of the leading two answers.
And, while waiting for more answers, image credit goes to Bandara H et al, from their article in the curiously named
"International Journal of Recent Scientific Research".
Presumably earlier volumes of the Journal get renamed progressively as time passes?
"International Journal of Recent Scientific Research".
Presumably earlier volumes of the Journal get renamed progressively as time passes?
Now that someone has answered "Must not stent" to Scenario B, I can ask Scenario C.
This time, you don& #39;t measure FFR. They clearly meet PCI criteria, so no need.
But you are an ORBITA investigator. @rallamee is hiding under the drapes, and jumps up and hits you with a mallet.
*She* measures the FFR, but doesn& #39;t tell you the result.
But you are an ORBITA investigator. @rallamee is hiding under the drapes, and jumps up and hits you with a mallet.
*She* measures the FFR, but doesn& #39;t tell you the result.
Once you regain consciousness, @rallamee is nowhere to be seen, and nobody around you knows what the FFR is.
(It happens to be 0.85, but nobody knows that.)
All you know is, 58yo M, angina, that& #39;s the angiogram, stress echo positive.
Can you now randomize?
(It happens to be 0.85, but nobody knows that.)
All you know is, 58yo M, angina, that& #39;s the angiogram, stress echo positive.
Can you now randomize?
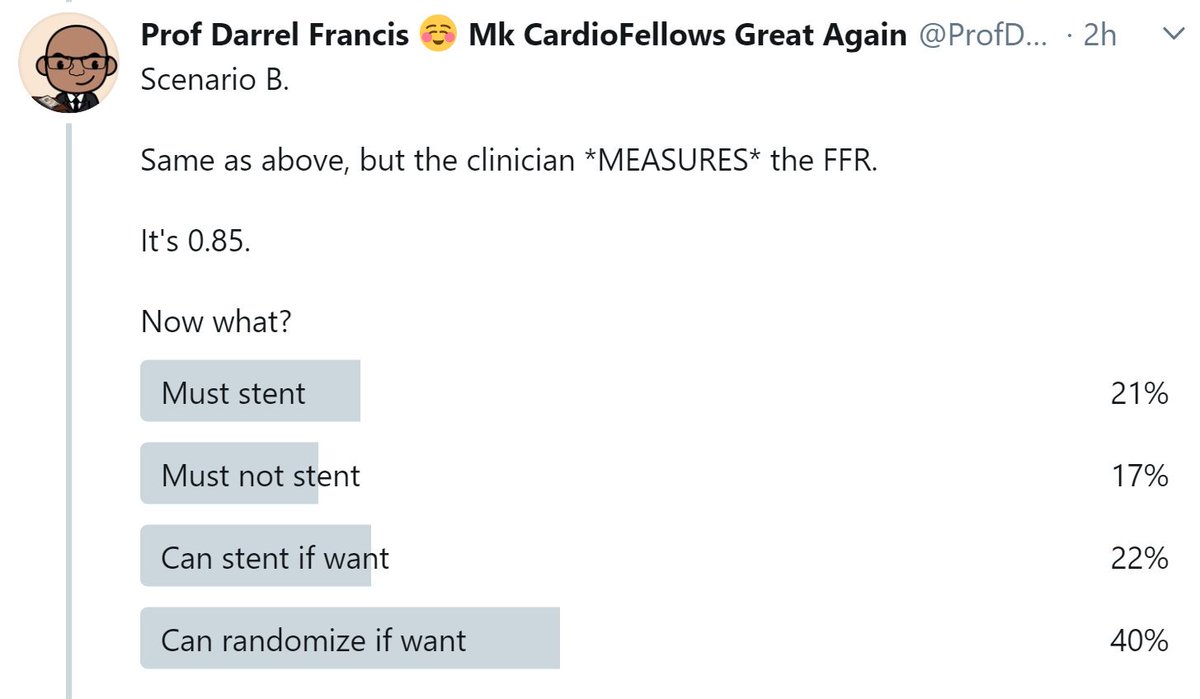
In Scenario B, here are the scores so far.
Remember, this is for a patient with Angina, a positive stress echo, the angiogram above, and a clinically measured (i.e. available to the operator) FFR of 0.85.
Remember, this is for a patient with Angina, a positive stress echo, the angiogram above, and a clinically measured (i.e. available to the operator) FFR of 0.85.
In the above result, what proportion of respondents, are ABSOLUTELY CERTAIN that there is only one correct course of action (stent versus no stent)?
Wonderful that so many people are certain, isn& #39;t it?
(The only fly in the ointment is that they are certain, in approximately equal numbers, of completely opposite truths.)
(The only fly in the ointment is that they are certain, in approximately equal numbers, of completely opposite truths.)
I believe the "must stent" people are feeling that if you DON& #39;T know the FFR, then as far as you are concerned, there is symptoms + obvious lesion + ischaemia on stress echo, and this equals stent.
I think I understand how they feel.
I think I understand how they feel.
Meanwhile, I believe the "must not stent" people are feeling that *even if THE OPERATOR does not know the FFR*, the FFR is indeed non-significant, so the operator (in some sense) "must" not stent.
I think I understand how they feel too.
I think I understand how they feel too.
I could summarise their view as:
"If my house is on fire, does the fact that I don& #39;t know about, mean that my house is not on fire? Of course not. It& #39;s still on fire."
"If my house is on fire, does the fact that I don& #39;t know about, mean that my house is not on fire? Of course not. It& #39;s still on fire."
But then I ask the question that got me shunned at the British Cardiovascular Intervention Society.
This here lesion:
This here lesion:
At 13:52 hrs on Tuesday, @rallamee measured its FFR.
The lesion& #39;s FFR was 0.85.
At 13:50, i.e. before she made the measurement, what was the lesion& #39;s FFR?
The lesion& #39;s FFR was 0.85.
At 13:50, i.e. before she made the measurement, what was the lesion& #39;s FFR?
And there we have it. *That* is the source of the debate!
EXACTLY @SorenK!
The ESC tells us to measure FFR if you are not sure what to do. This is good advice, since it allows you to go forward instead of hesitating in indecision. Equally, you could toss a coin, or inspect the entrails of a passing bird.
The ESC tells us to measure FFR if you are not sure what to do. This is good advice, since it allows you to go forward instead of hesitating in indecision. Equally, you could toss a coin, or inspect the entrails of a passing bird.
What the authors of the Medscape Complaint, and the panelists at BCIS, seem to be unable to understand, is that
"When you don& #39;t know what to do, do FFR"
is *not* the same as
"ONLY when you don& #39;t know what to do, do FFR".
"When you don& #39;t know what to do, do FFR"
is *not* the same as
"ONLY when you don& #39;t know what to do, do FFR".
So when a patient is clinically eligible for PCI based on angina + positive ischaemia test + convincing angiogram, they are happy to do PCI.
But when they later discover that a "secret" FFR was done, and was negative, the circuits in their brains start giving out sparks.
"FFRs are only done when there is uncertainty, so a mild FFR means do not stent."
"Yet they stented!"
"Does not compute?!?!"
"ERROR @!@!@! ERROR!"
"FFRs are only done when there is uncertainty, so a mild FFR means do not stent."
"Yet they stented!"
"Does not compute?!?!"
"ERROR @!@!@! ERROR!"
They absolutely do not understand that the FFR was measured and kept out of sight of the interventional operator, to *prevent* panic and extistential crisis when an operator finds that a convincing lesion, angina, and positive stress echo, can coincide with FFR that looks mild.
I don& #39;t blame them for not understanding stuff.
There& #39;s plenty of stuff I don& #39;t understand.
But I don& #39;t write letters to Medscape, advertising the fact that I don& #39;t understand the stuff I write guidelines about!
I keep my un-understanding to myself.
There& #39;s plenty of stuff I don& #39;t understand.
But I don& #39;t write letters to Medscape, advertising the fact that I don& #39;t understand the stuff I write guidelines about!
I keep my un-understanding to myself.
And some closing thoughts. Remember how the guidelines have swallowed the FFR dictum, hook, line and sinker?
When you are uncertain of a lesion, they tell you to measure FFR?
"Don& #39;t judge by eye? Appearances can be deceptive, blah blah blah?"
When you are uncertain of a lesion, they tell you to measure FFR?
"Don& #39;t judge by eye? Appearances can be deceptive, blah blah blah?"
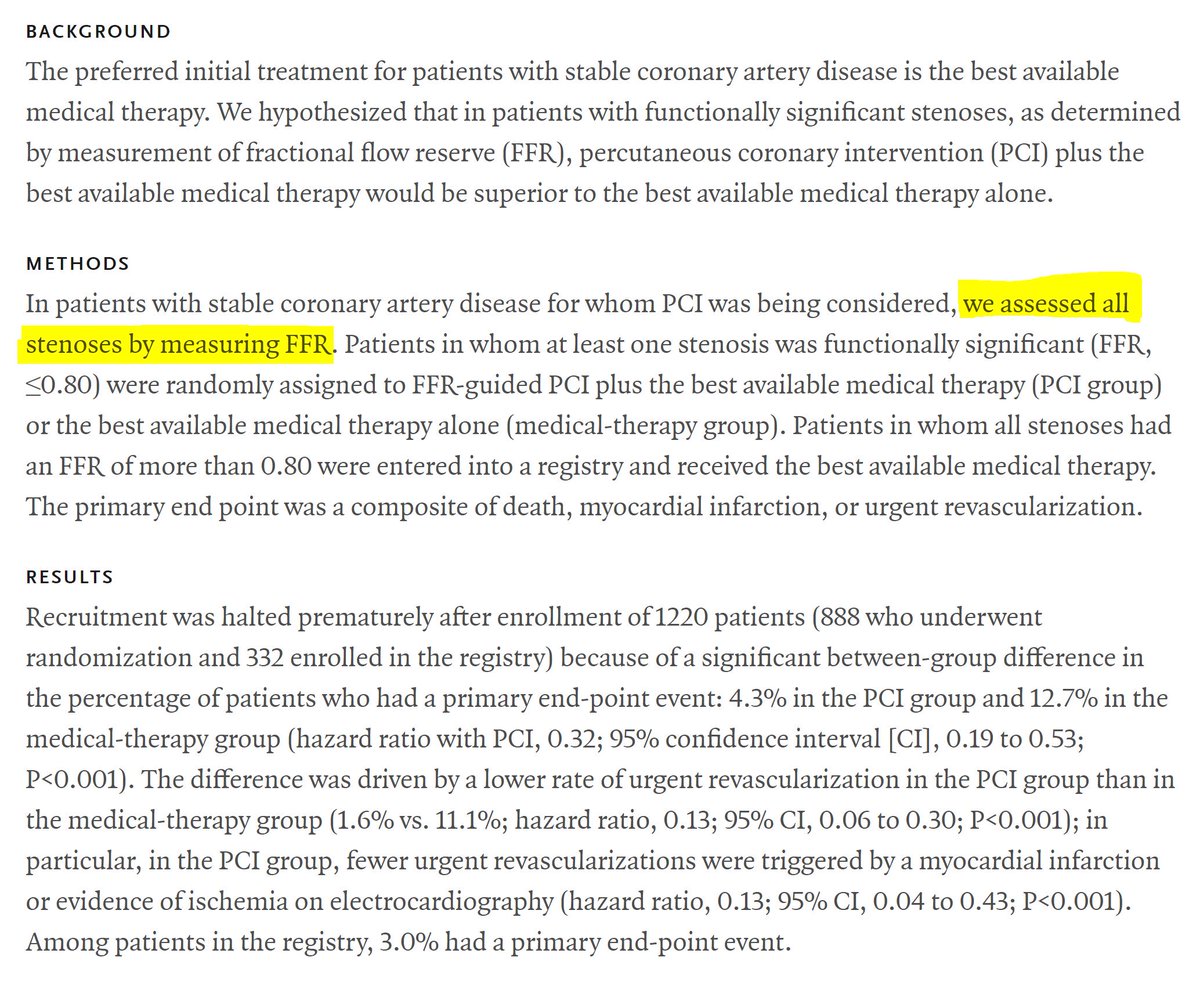
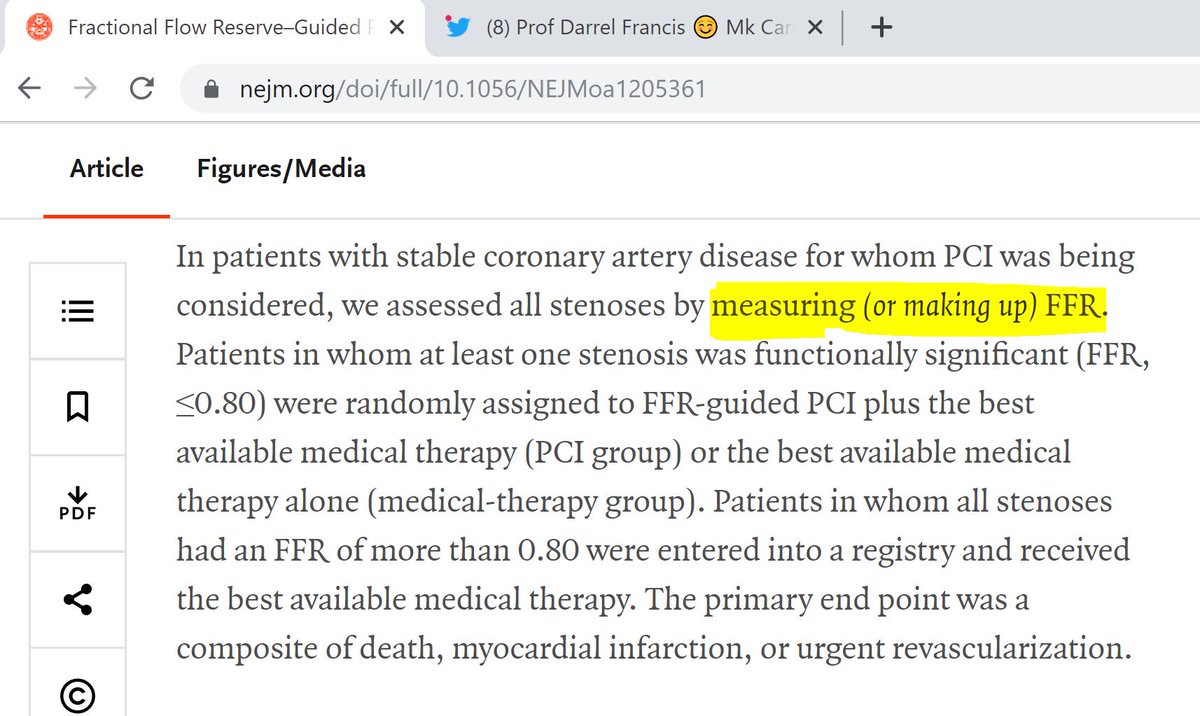
This is based on FAME-2.
Here is a reminder of the paper, which you can read for free by googling for NEJMoa1205361:
Here is a reminder of the paper, which you can read for free by googling for NEJMoa1205361:
"... by measuring FFR."
And that is why the ESC encourage us to do this. But how is FFR measured?
And that is why the ESC encourage us to do this. But how is FFR measured?
After FAME 2 was published in 2012, most people took the abstract at face value, and assumed that "measured FFR" meant "measured FFR using a pressure wire".
In 2018, it emerged that 133 of the FFR measurements were made up, as "0.5". ( #article_letters">https://www.nejm.org/doi/full/10.1056/NEJMoa1803538 #article_letters)
So">https://www.nejm.org/doi/full/... the advice to "measure FFR" would be better worded:
"Measure or make up FFR".
So">https://www.nejm.org/doi/full/... the advice to "measure FFR" would be better worded:
"Measure or make up FFR".
Brahmajee Nallamothu @bnallamo and I enquired what the results were in the patients in whom all FFRs were truly measured as written in the Abstract, rather than made up.
*Either* the authors did not understand the question
*Or* they assumed that readers were too stupid to notice they hadn& #39;t answered that question.
Regardless of the reason, they made up (and answered) a different question.
*Or* they assumed that readers were too stupid to notice they hadn& #39;t answered that question.
Regardless of the reason, they made up (and answered) a different question.
Anyway, the end result of this is a second reason for me to reject the reasoning of the ESC Complaint Letter to Medscape.
Not only is their reasoning (to put it kindly) faulty,
But the trial on which they rely is more problematic and secretive than they realise.
Not only is their reasoning (to put it kindly) faulty,
But the trial on which they rely is more problematic and secretive than they realise.
Brilliantly asked David!
"Functionally significant" is a made-up concept for sloppy speakers.
We use the term when we want listeners to THINK they have understood what we have said, but for us to be able to slip out of any particular meaning of it.
"Functionally significant" is a made-up concept for sloppy speakers.
We use the term when we want listeners to THINK they have understood what we have said, but for us to be able to slip out of any particular meaning of it.
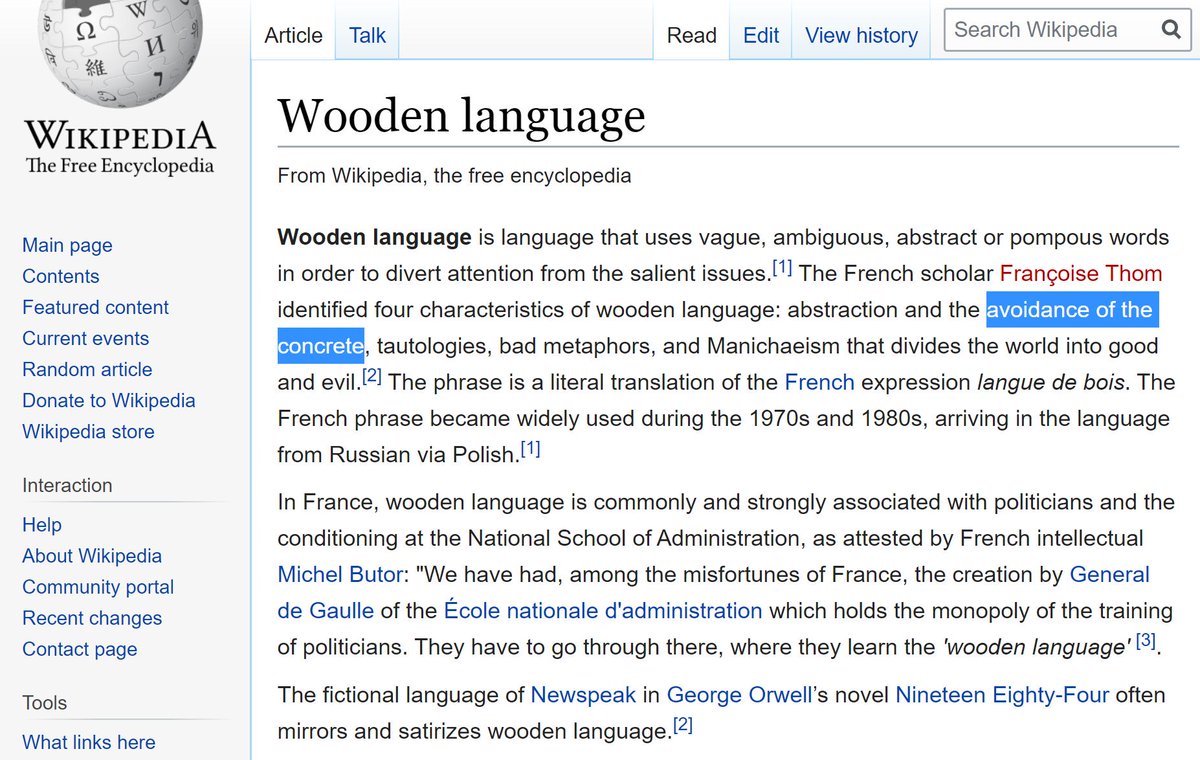
Whenever I hear the words "functionally significant", that picture goes through my mind.
Wikipedia, inevitably, has a name for it.
Wikipedia, inevitably, has a name for it.
When ORBITA-HQ fellows try to put such slippery terminology into a paper, I mock them remorselessly.
Eventually they learn to avoid the shame by simply saying what they mean.
Eventually they learn to avoid the shame by simply saying what they mean.
Examples are:
"Stress echo positive", or
"FFR positive", or
"Causing angina", or
"Causing ST depression on Ex ECG", or
"Any of the above", or
"Any of the above, excluding & #39;causing angina& #39;"
"Stress echo positive", or
"FFR positive", or
"Causing angina", or
"Causing ST depression on Ex ECG", or
"Any of the above", or
"Any of the above, excluding & #39;causing angina& #39;"
Venk Murthy @venkmurthy raises the point that the poor old FAME-2 team were having a bad-hair day when doing their calculations for their 2018 Circ paper. https://twitter.com/venkmurthy/status/1193318138189959170">https://twitter.com/venkmurth...
I don& #39;t mind that so much, because they did go back and correct the amusing goofs.
We all make mistakes. As long as we correct them promptly and clearly, I tend to say it& #39;s OK.
We all make mistakes. As long as we correct them promptly and clearly, I tend to say it& #39;s OK.
A bigger problem is when we make mistakes and DON& #39;T correct them.
Sometimes it is because it wasn& #39;t a mistake at all, but an intent to mislead.
Sometimes it is because it wasn& #39;t a mistake at all, but an intent to mislead.
NEJM generally doesn& #39;t insist on correcting mistakes.
For example, they still haven& #39;t _retracted_ the famously fictitious DECREASE trial of Don Poldermans, the jolly japester of perioperative care.
I& #39;ve argued with them tediuously, but failed.
For example, they still haven& #39;t _retracted_ the famously fictitious DECREASE trial of Don Poldermans, the jolly japester of perioperative care.
I& #39;ve argued with them tediuously, but failed.
So I don& #39;t expect them to correct the FAME-2 abstract either.
Therefore we are going to just have to mentally correct it, and tell guideline-writers too, since they also may be relying on the abstract to be truthful.
Therefore we are going to just have to mentally correct it, and tell guideline-writers too, since they also may be relying on the abstract to be truthful.
So here is my contribution on the subject. Show this whenever anyone tries to lecture you on FFR, or tries to tell you what to do in general.
If anyone tries to tell you to measure FFR, tell them you are exercising your right to make up the value as 0.5.
If, for some reason, you DO measure FFR, and don& #39;t want to do what it tells you to do, ask them this:
"In this patient, I have measured (not made up) the FFR values.
In FAME-2, what was the result within the subgroup matching mine, i.e. in patients where all the FFRs were measured, not made up?"
In FAME-2, what was the result within the subgroup matching mine, i.e. in patients where all the FFRs were measured, not made up?"

 Read on Twitter
Read on Twitter