Here we go. My first #medtwitter #tweetorial. A subject near and dear to my heart. Venous air embolism.
If I have an IV line and someone injects air into it, how much will it take to kill me?
#FOAMed #FOAMrad
1/
If I have an IV line and someone injects air into it, how much will it take to kill me?
#FOAMed #FOAMrad
1/
This 2001 paper from the journal Anesthesiology puts the amount of air needed to kill at 200-300 mL or 3-5 mL/kg.
https://www.ncbi.nlm.nih.gov/pubmed/11176104/
2/">https://www.ncbi.nlm.nih.gov/pubmed/11...
https://www.ncbi.nlm.nih.gov/pubmed/11176104/
2/">https://www.ncbi.nlm.nih.gov/pubmed/11...
But where is that air probably going to be when it kills you?
3/
3/
Probably the heart, can you be more specific?
4/
4/
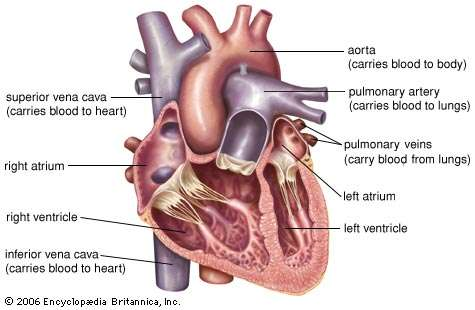
Follow up question, what is the anterior-most chamber of the heart?
5/
5/
Anterior-most chamber of the heart is right ventricle. Here& #39;s an axial CT image of an air embolism with air in right ventricle. (credit https://coreem.net/core/air-embolism/)
6/">https://coreem.net/core/air-...
6/">https://coreem.net/core/air-...
So clinical scenario, you& #39;re pulling out a central line. The patient takes in a breath while you& #39;re pulling the catheter. Then they go into PEA arrest. You call a code, put the patient on 100% oxygen non-rebreather face mask, what position should the patient be in?
7/
7/
Left lateral decubitus position is the answer. But first we have to understand why the patient is in PEA arrest and why it takes so much air to kill.
For most people, it has to be enough air to fill up the right ventricle and pulmonary outflow tract.
8/
For most people, it has to be enough air to fill up the right ventricle and pulmonary outflow tract.
8/
A little bit of venous air is fine. Fairly common to see incidental air bubbles in right ventricle or pulmonary artery when reading chest CTs. It goes to the pulmonary arteries, goes to the alveoli and you breathe it out.
9/
9/
When I place IVC filters in patients who can& #39;t tolerate iodinated contrast, I inject a 60 mL bolus of CO2 directly into the IVC for the venogram. Patients do just fine.
10/
10/
The reason it takes so much air to kill is that the air needs to completely fill the right ventricle. Enough air to break the circuit of fluid. Since air compresses more than blood, the RV will be contracting the air bubble leading to "vapor lock" and cardiovascular collapse.
11/
11/
Going back to the clinical scenario of PEA arrest and air embolism. You want to have the air float away from the right ventricle and have blood flow into the RV to re-establish the circuit of fluid. Left lateral decub position raises the SVC and IVC above the RV.
12/
12/
If you get the circuit of fluid going again, forward flow of blood will get the air bubbles going to pulmonary circulation where the air can get across the alveoli.
13/
13/
Last ditch effort, take a big needle and a big syringe, go subxiphoid into the RV and aspirate the air. (Hopefully you never have to do this)
14/
14/
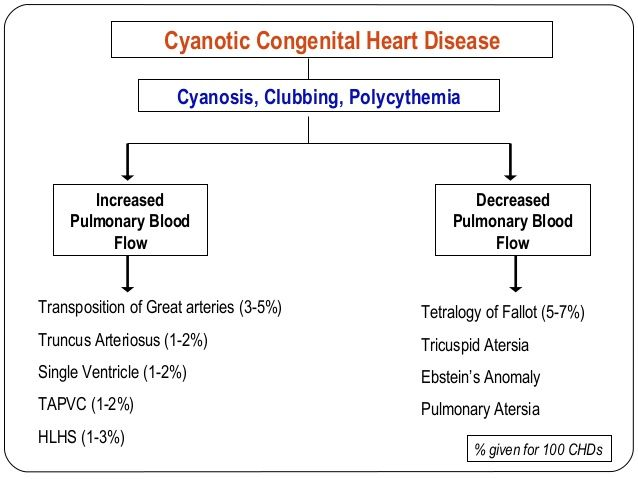
So what about PFO, ASD, VSD. Should we worry about those patients? Probably not, left side pressures are so much greater than right side. Would be hard to imagine air getting across to arterial circulation outside of Eisenmenger syndrome.
15/
15/
Pulmonary AV malformation / AV fistula. That& #39;s the one patient population where only a few mL of air could kill you.
If the air manages to make it to a PAVM and bypasses the alveoli, conceivably a tiny bubble could make it to a cerebral artery or coronary artery and kill.
16/
If the air manages to make it to a PAVM and bypasses the alveoli, conceivably a tiny bubble could make it to a cerebral artery or coronary artery and kill.
16/
So a little air in the line going to the peripheral IV, probably not a big deal.
When to worry? Patients with central lines. Don& #39;t leave them uncapped, deep breath could pull in enough air. Same thing when placing and removing.
17/
When to worry? Patients with central lines. Don& #39;t leave them uncapped, deep breath could pull in enough air. Same thing when placing and removing.
17/
Also, if you& #39;re going to a code in the CT scanner. Check the power injector. If the tech never loaded contrast, there& #39;s another time that a large bolus of air could conceivably be injected to the vein.
18/
18/
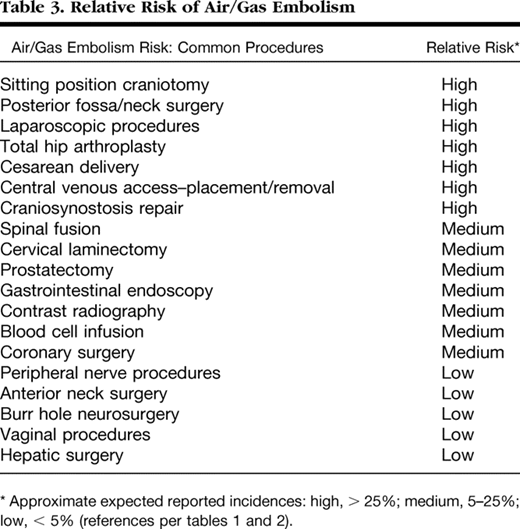
Here& #39;s a list of procedures and risks of air embolism from a journal Anesthesiology article from 2007.
https://anesthesiology.pubs.asahq.org/article.aspx?articleid=1923071
19/">https://anesthesiology.pubs.asahq.org/article.a...
https://anesthesiology.pubs.asahq.org/article.aspx?articleid=1923071
19/">https://anesthesiology.pubs.asahq.org/article.a...
Going back to right-to-left shunt. I mentioned Eisenmenger Syndrome and PAVM. That& #39;s for adults.
Neonates with cyanotic heart disease are cyanotic because of a right to left shunt. A few drops of venous air could be fatal for them as well.
20/
Neonates with cyanotic heart disease are cyanotic because of a right to left shunt. A few drops of venous air could be fatal for them as well.
20/

 Read on Twitter
Read on Twitter