1/
Why do some people treat B12 deficiency with oral B12 even if the problem is poor absorption?
Is this a good idea? Is it a paradox? Let’s reconcile, @tonybrue #tweetorial style.
Why do some people treat B12 deficiency with oral B12 even if the problem is poor absorption?
Is this a good idea? Is it a paradox? Let’s reconcile, @tonybrue #tweetorial style.
2/
First, a question:
A previously healthy woman has a hemoglobin of 11, MCV 99, B12 138, and + anti-parietal cell antibody. How would you typically treat her?
First, a question:
A previously healthy woman has a hemoglobin of 11, MCV 99, B12 138, and + anti-parietal cell antibody. How would you typically treat her?
3/
I recommend D.
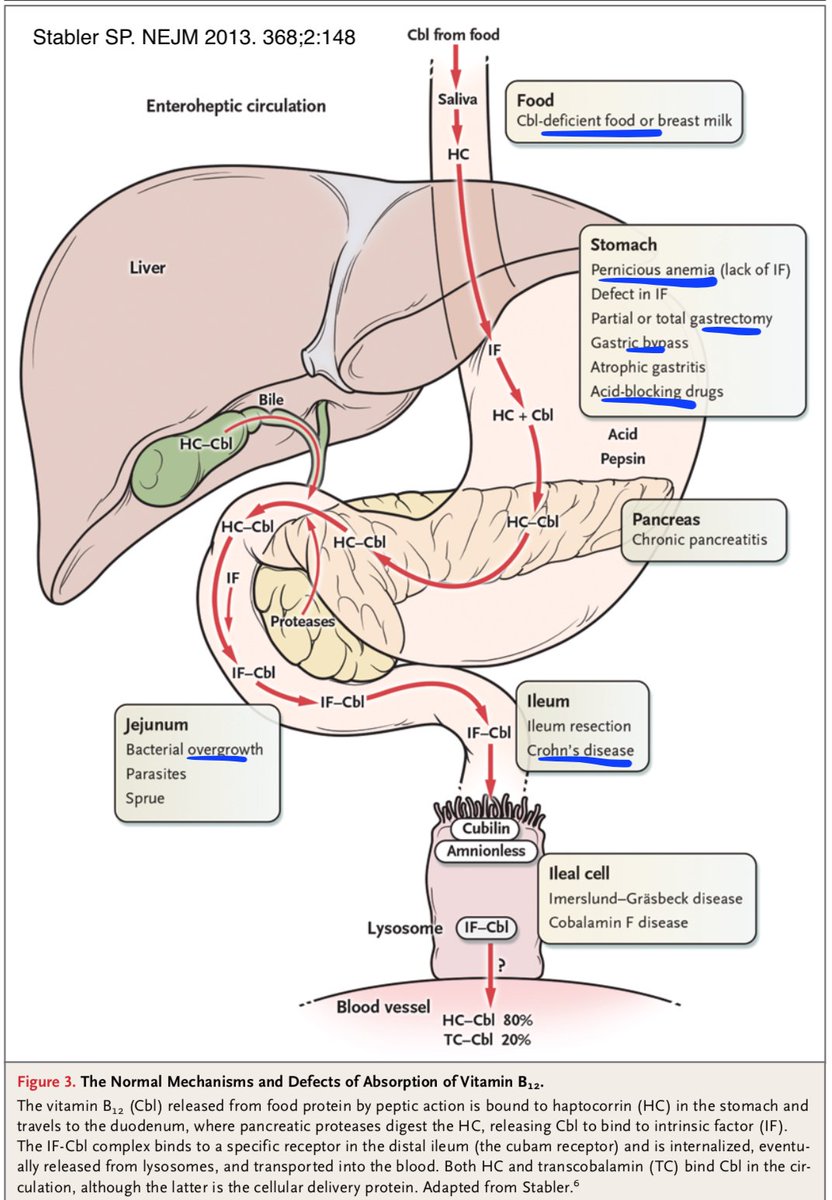
Let’s start by looking at the causes of B12 deficiency. This great diagram shows normal absorption and outlines most possible causes. At the top is a B12-deficient diet. But the rest involve some mechanism of not absorbing.
I recommend D.
Let’s start by looking at the causes of B12 deficiency. This great diagram shows normal absorption and outlines most possible causes. At the top is a B12-deficient diet. But the rest involve some mechanism of not absorbing.
4/
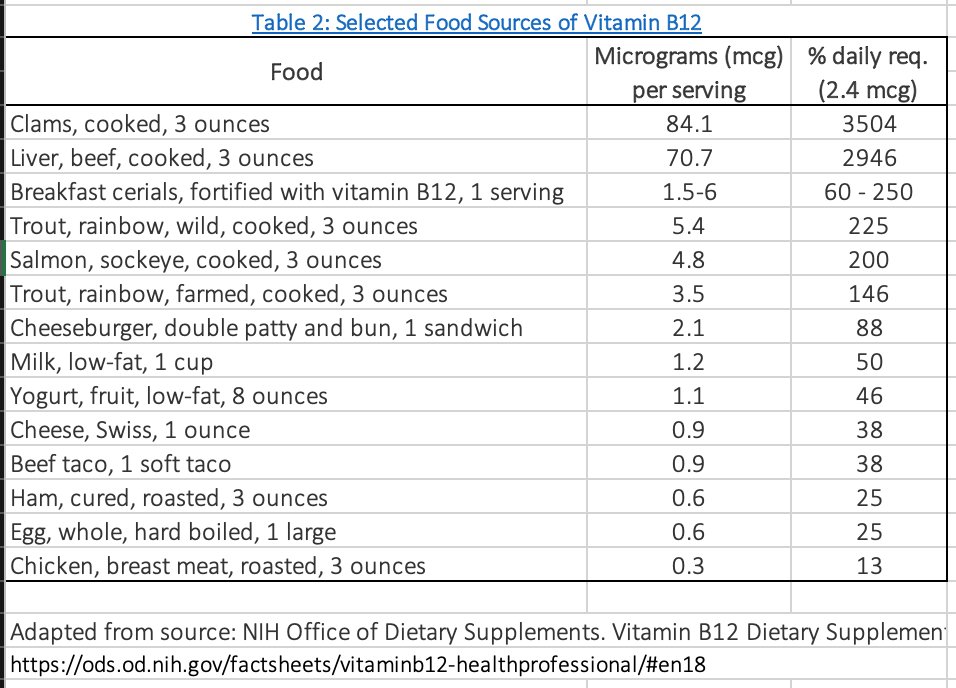
Now take a look at B12 content of these foods. Basically, if you’re not vegan, it’s hard to eat a “B12-deficient diet.” (And as opposed to thiamine, where you can run out of stores in days-weeks of malnutrition, the liver’s B12 stores last at least many months).
Now take a look at B12 content of these foods. Basically, if you’re not vegan, it’s hard to eat a “B12-deficient diet.” (And as opposed to thiamine, where you can run out of stores in days-weeks of malnutrition, the liver’s B12 stores last at least many months).
5/
So if most B12 deficiency is malabsorptive, why would PO supplementation work? Well, absorption is not binary. And when something impairs the mechanisms of absorption, it’s the % absorbed that is reduced.
So if most B12 deficiency is malabsorptive, why would PO supplementation work? Well, absorption is not binary. And when something impairs the mechanisms of absorption, it’s the % absorbed that is reduced.
6/
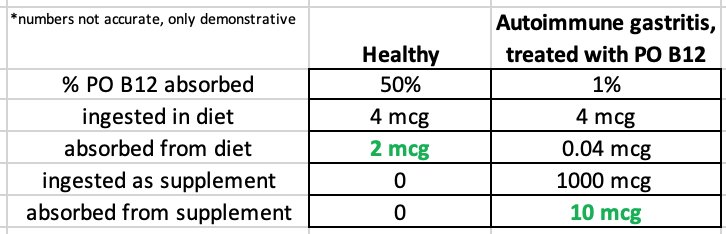
Let’s ballpark some numbers. I’m healthy, and I ingest about 4 mcg B12. I have normal intrinsic factor and ileum, so I absorb 50% of it, or 2 mcg.
Let’s ballpark some numbers. I’m healthy, and I ingest about 4 mcg B12. I have normal intrinsic factor and ileum, so I absorb 50% of it, or 2 mcg.
7/
But even if I lose my intrinsic factor (pernicious anemia, gastric bypass, etc) or ileum (resection, Crohn’s, etc), there& #39;s still SOME absorption - it doesn’t go to 0%. Thus it can be overcome with enough “substrate.” Ingest 1000 mcg and the 1% (10 mcg) absorbed is enough!
But even if I lose my intrinsic factor (pernicious anemia, gastric bypass, etc) or ileum (resection, Crohn’s, etc), there& #39;s still SOME absorption - it doesn’t go to 0%. Thus it can be overcome with enough “substrate.” Ingest 1000 mcg and the 1% (10 mcg) absorbed is enough!
8/
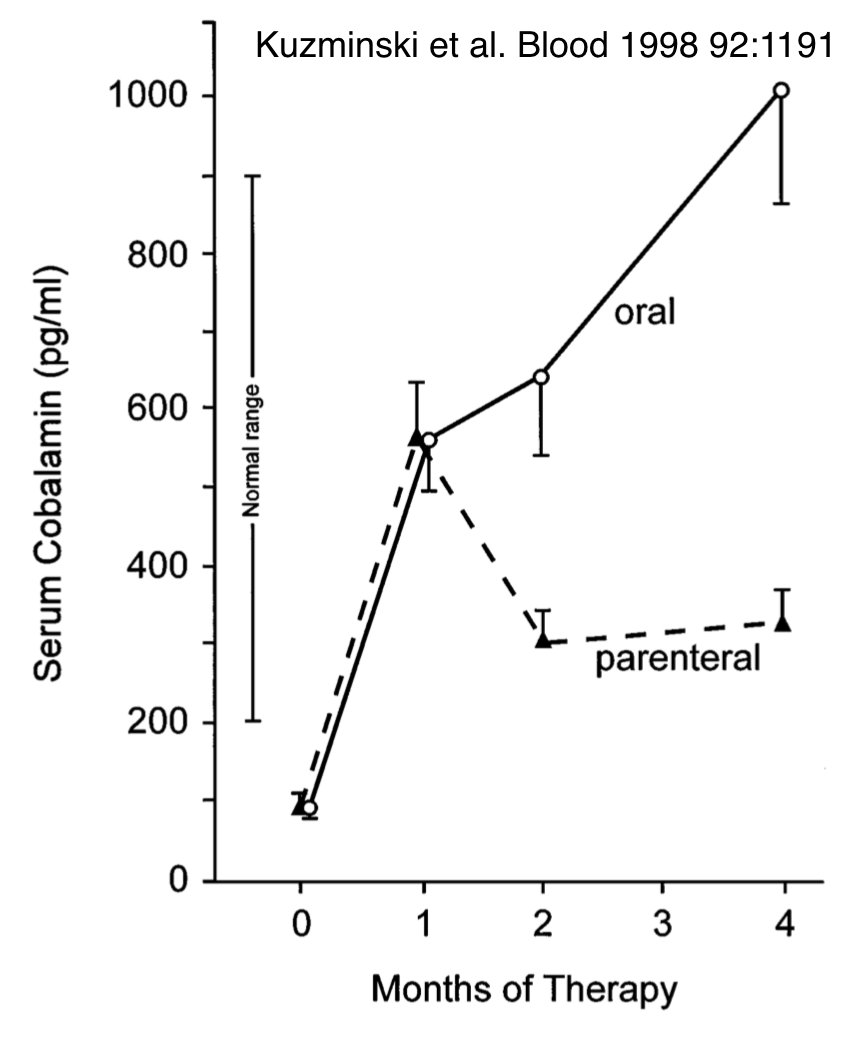
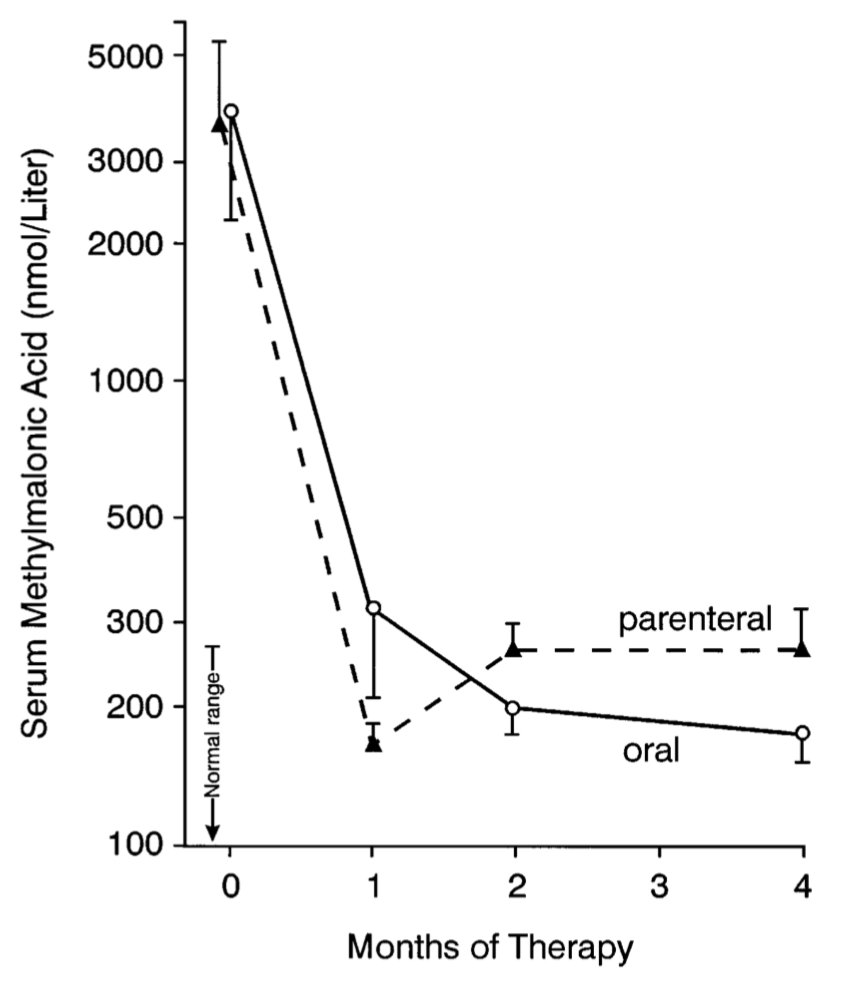
Great, should work in theory. Does it pan out in practice? In seminal Blood RCT, folks with significant B12 def got 1000 mcg IM monthly vs. 2000 mcg PO daily B12. Almost all people in PO group had pernicious anemia / atrophic gastritis (i.e. malabsorptive cause). Results:
Great, should work in theory. Does it pan out in practice? In seminal Blood RCT, folks with significant B12 def got 1000 mcg IM monthly vs. 2000 mcg PO daily B12. Almost all people in PO group had pernicious anemia / atrophic gastritis (i.e. malabsorptive cause). Results:
9/
B12 and methylmalonic acid response (surrogate for function) at least as good with PO. 2018 Cochrane review of 3 RCTs (including that one) similarly concluded equivalent efficacy. Most experts/guidelines endorse PO treatment as first line. https://bit.ly/2WlW9zx ">https://bit.ly/2WlW9zx&q...
B12 and methylmalonic acid response (surrogate for function) at least as good with PO. 2018 Cochrane review of 3 RCTs (including that one) similarly concluded equivalent efficacy. Most experts/guidelines endorse PO treatment as first line. https://bit.ly/2WlW9zx ">https://bit.ly/2WlW9zx&q...
10/
Couple extra B12 pearls before revisiting question and summarizing.
Couple extra B12 pearls before revisiting question and summarizing.
11/
“Borderline” B12 levels 200-350 are associated with elevated methylmalonic acid levels and symptoms/abnormalities of deficiency. If there are any compatible symptoms/findings – which I hope there were if level was being checked – just treat it as deficiency.
“Borderline” B12 levels 200-350 are associated with elevated methylmalonic acid levels and symptoms/abnormalities of deficiency. If there are any compatible symptoms/findings – which I hope there were if level was being checked – just treat it as deficiency.
12/
PPIs/H2Bs (acidity cleaves B12 from food) and metformin (impairs ileal absorption) can cause dose- and time-dependent reduction in B12 levels. @UpToDate summarizes the evidence beautifully if you want to read more:
PPIs/H2Bs (acidity cleaves B12 from food) and metformin (impairs ileal absorption) can cause dose- and time-dependent reduction in B12 levels. @UpToDate summarizes the evidence beautifully if you want to read more:
13/
Duration of treatment: most causes of B12 deficiency (e.g. pernicious anemia from the opening case) are not reversible. Treatment often gets stopped, and deficiency develops again. Instead, treat indefinitely, unless you have reversed the cause.
Duration of treatment: most causes of B12 deficiency (e.g. pernicious anemia from the opening case) are not reversible. Treatment often gets stopped, and deficiency develops again. Instead, treat indefinitely, unless you have reversed the cause.
14/
Let’s revisit:
A previously healthy woman has a hemoglobin of 11, MCV 99, B12 138, and + anti-parietal cell antibody. How would you typically treat her?
Let’s revisit:
A previously healthy woman has a hemoglobin of 11, MCV 99, B12 138, and + anti-parietal cell antibody. How would you typically treat her?
15/
Important caveat: if someone is having significant neurologic symptoms from B12 deficiency, it’s recommended to have a couple IM doses in a row (even daily) before transitioning. This makes sense to me.
Important caveat: if someone is having significant neurologic symptoms from B12 deficiency, it’s recommended to have a couple IM doses in a row (even daily) before transitioning. This makes sense to me.
16/
Take-home points:
- Most B12 deficiency is a problem with absorption
- This reduction in % absorbed can be overcome with high PO dose
- 1000 mcg PO daily indefinitely is right for most – it is as effective and easier/less costly than shots
Thanks for reading!
Take-home points:
- Most B12 deficiency is a problem with absorption
- This reduction in % absorbed can be overcome with high PO dose
- 1000 mcg PO daily indefinitely is right for most – it is as effective and easier/less costly than shots
Thanks for reading!

 Read on Twitter
Read on Twitter