1/
Why is tricuspid valve (TV) endocarditis more common in those who use intravenous drugs?
The portal of entry for most bacteria is the venous system. If quick access to the right-heart were enough, TV endocarditis would be more common in everyone.
There must be more to it...
Why is tricuspid valve (TV) endocarditis more common in those who use intravenous drugs?
The portal of entry for most bacteria is the venous system. If quick access to the right-heart were enough, TV endocarditis would be more common in everyone.
There must be more to it...
2/
In order to understand why the tricuspid valve is more commonly affected in those with IVDU, it is essential to first understand the pathogenesis of infective endocarditis.
So, a question: which of the following confers the greatest risk of infective endocarditis?
In order to understand why the tricuspid valve is more commonly affected in those with IVDU, it is essential to first understand the pathogenesis of infective endocarditis.
So, a question: which of the following confers the greatest risk of infective endocarditis?
3/
Next, let& #39;s confirm that, in all comers, tricuspid valve involvement is relatively infrequent in infective endocarditis. One study reported the following rates:
35% aortic
29% mitral
14% aortic & mitral
9% tricuspid
1% pulmonic
2% left & right
https://www.ncbi.nlm.nih.gov/pubmed/12090865 ">https://www.ncbi.nlm.nih.gov/pubmed/12...
Next, let& #39;s confirm that, in all comers, tricuspid valve involvement is relatively infrequent in infective endocarditis. One study reported the following rates:
35% aortic
29% mitral
14% aortic & mitral
9% tricuspid
1% pulmonic
2% left & right
https://www.ncbi.nlm.nih.gov/pubmed/12090865 ">https://www.ncbi.nlm.nih.gov/pubmed/12...
4/
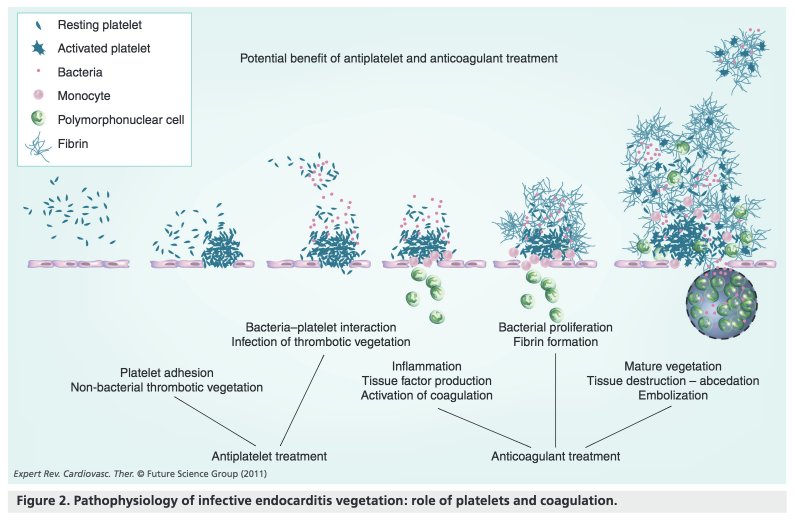
At least three steps are required for infective endocarditis (IE) to occur.
1. Endothelial injury
2. Activation of hemostasis with thrombus formation (i.e., nonbacterial thrombotic endocarditis, NBTE)
3. Secondary bacterial infection (i.e., IE)
https://www.ncbi.nlm.nih.gov/pubmed/4014276 ">https://www.ncbi.nlm.nih.gov/pubmed/40...
At least three steps are required for infective endocarditis (IE) to occur.
1. Endothelial injury
2. Activation of hemostasis with thrombus formation (i.e., nonbacterial thrombotic endocarditis, NBTE)
3. Secondary bacterial infection (i.e., IE)
https://www.ncbi.nlm.nih.gov/pubmed/4014276 ">https://www.ncbi.nlm.nih.gov/pubmed/40...
5/
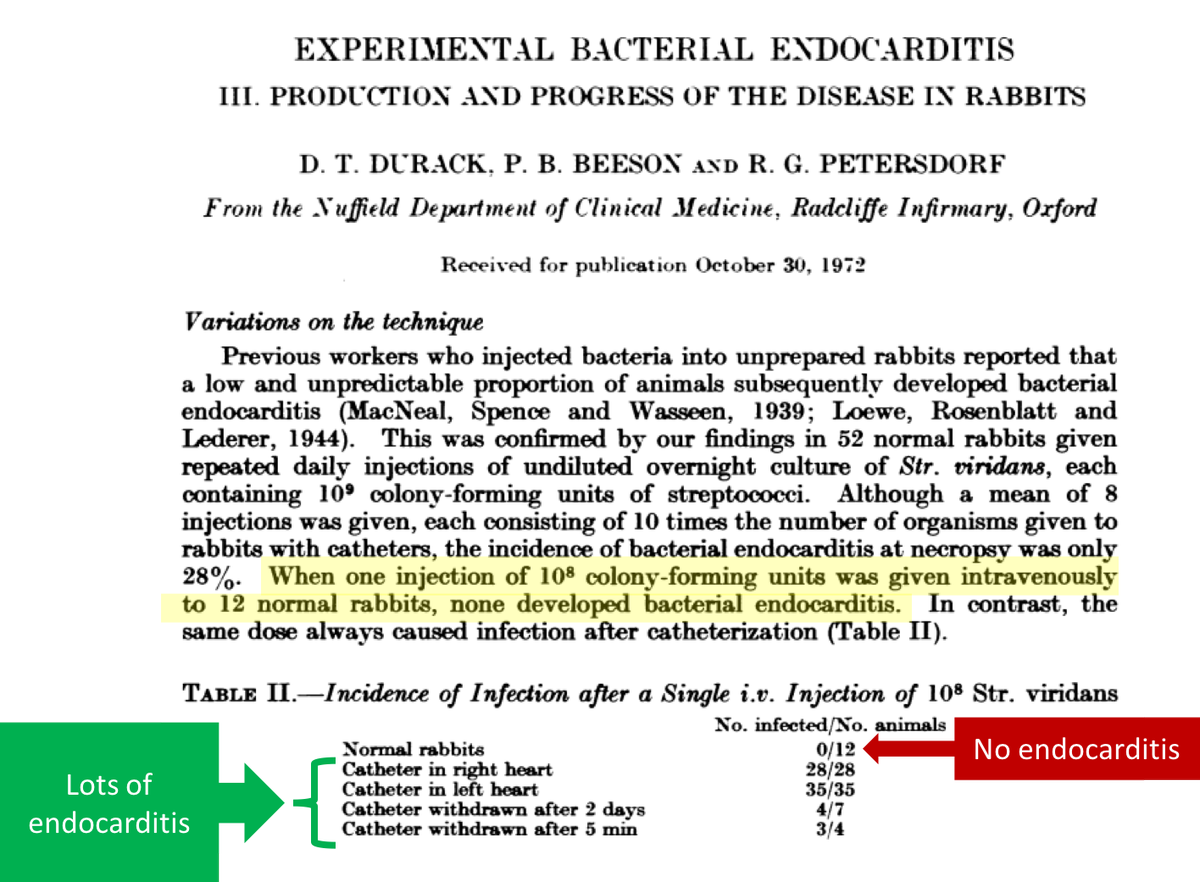
Regarding 1, vegetations rarely form on intact endothelium.
In the 1970s, Durack injected bacteria into rabbits. Some had catheter trauma (disrupting the endothelium); others did not. Results:
*no endothelial injury = no IE
*endothelial injury = IE
https://www.ncbi.nlm.nih.gov/pubmed/4700697 ">https://www.ncbi.nlm.nih.gov/pubmed/47...
Regarding 1, vegetations rarely form on intact endothelium.
In the 1970s, Durack injected bacteria into rabbits. Some had catheter trauma (disrupting the endothelium); others did not. Results:
*no endothelial injury = no IE
*endothelial injury = IE
https://www.ncbi.nlm.nih.gov/pubmed/4700697 ">https://www.ncbi.nlm.nih.gov/pubmed/47...
6/
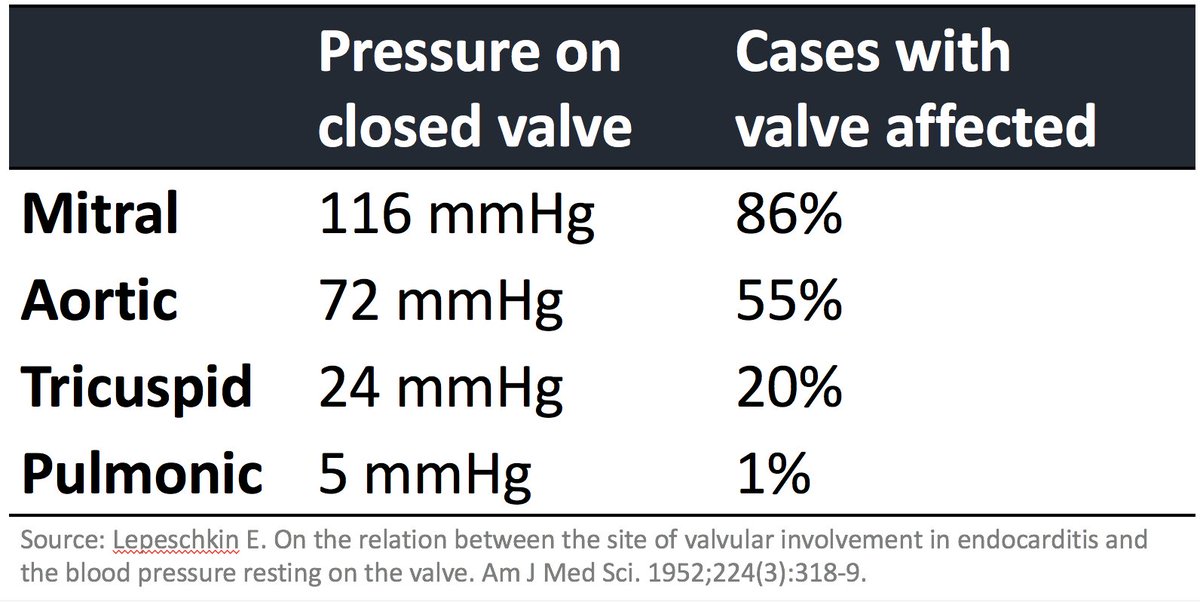
Endothelial injury is more likely in areas of high pressure as this creates shear stress and disruption of the endothelium.
In 1952, Lepeschkin correlated the pressure resting on a closed valve with rates of IE.
higher pressure = higher rate of IE
https://www.ncbi.nlm.nih.gov/pubmed/14952510 ">https://www.ncbi.nlm.nih.gov/pubmed/14...
Endothelial injury is more likely in areas of high pressure as this creates shear stress and disruption of the endothelium.
In 1952, Lepeschkin correlated the pressure resting on a closed valve with rates of IE.
higher pressure = higher rate of IE
https://www.ncbi.nlm.nih.gov/pubmed/14952510 ">https://www.ncbi.nlm.nih.gov/pubmed/14...
7/
The result of endothelial injury is activation of the clotting cascade and creation of thrombus. Other factors fuel thrombus formation:
*high shear stress https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> platelet activation
https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> platelet activation
*S aureus production of coagulase which converts fibrinogen to fibrin
https://www.ncbi.nlm.nih.gov/pubmed/21932963 ">https://www.ncbi.nlm.nih.gov/pubmed/21...
The result of endothelial injury is activation of the clotting cascade and creation of thrombus. Other factors fuel thrombus formation:
*high shear stress
*S aureus production of coagulase which converts fibrinogen to fibrin
https://www.ncbi.nlm.nih.gov/pubmed/21932963 ">https://www.ncbi.nlm.nih.gov/pubmed/21...
8/
Given the above, which of the following might be used to prevent infective endocarditis?
Given the above, which of the following might be used to prevent infective endocarditis?
9/
Both antiplatelets and anticoagulants have been suggested to prevent and/or treat IE.
The hypothesis: if we can reduce thrombus formation, maybe we can reduce infected vegetation formation and/or hasten resolution.
Both antiplatelets and anticoagulants have been suggested to prevent and/or treat IE.
The hypothesis: if we can reduce thrombus formation, maybe we can reduce infected vegetation formation and/or hasten resolution.
10/
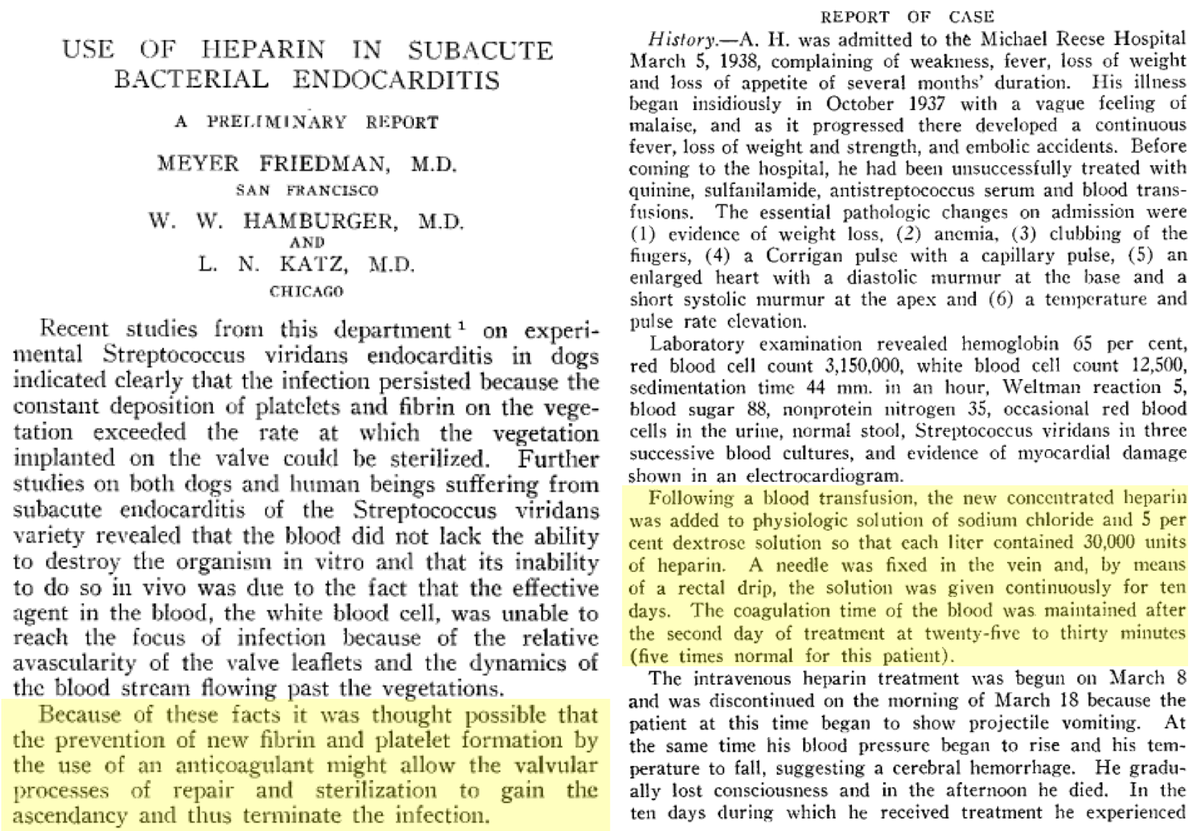
As far back as the 1930s, heparin was tried as treatment for IE. Recall that this predates penicillins. The linked case report by Friedman is an example of what was used to treat IE:
Sulfanilamide
Quinine
Antistrep serum
Adding heparin didn& #39;t work.
https://jamanetwork.com/journals/jama/article-abstract/1158756">https://jamanetwork.com/journals/...
As far back as the 1930s, heparin was tried as treatment for IE. Recall that this predates penicillins. The linked case report by Friedman is an example of what was used to treat IE:
Sulfanilamide
Quinine
Antistrep serum
Adding heparin didn& #39;t work.
https://jamanetwork.com/journals/jama/article-abstract/1158756">https://jamanetwork.com/journals/...
11/
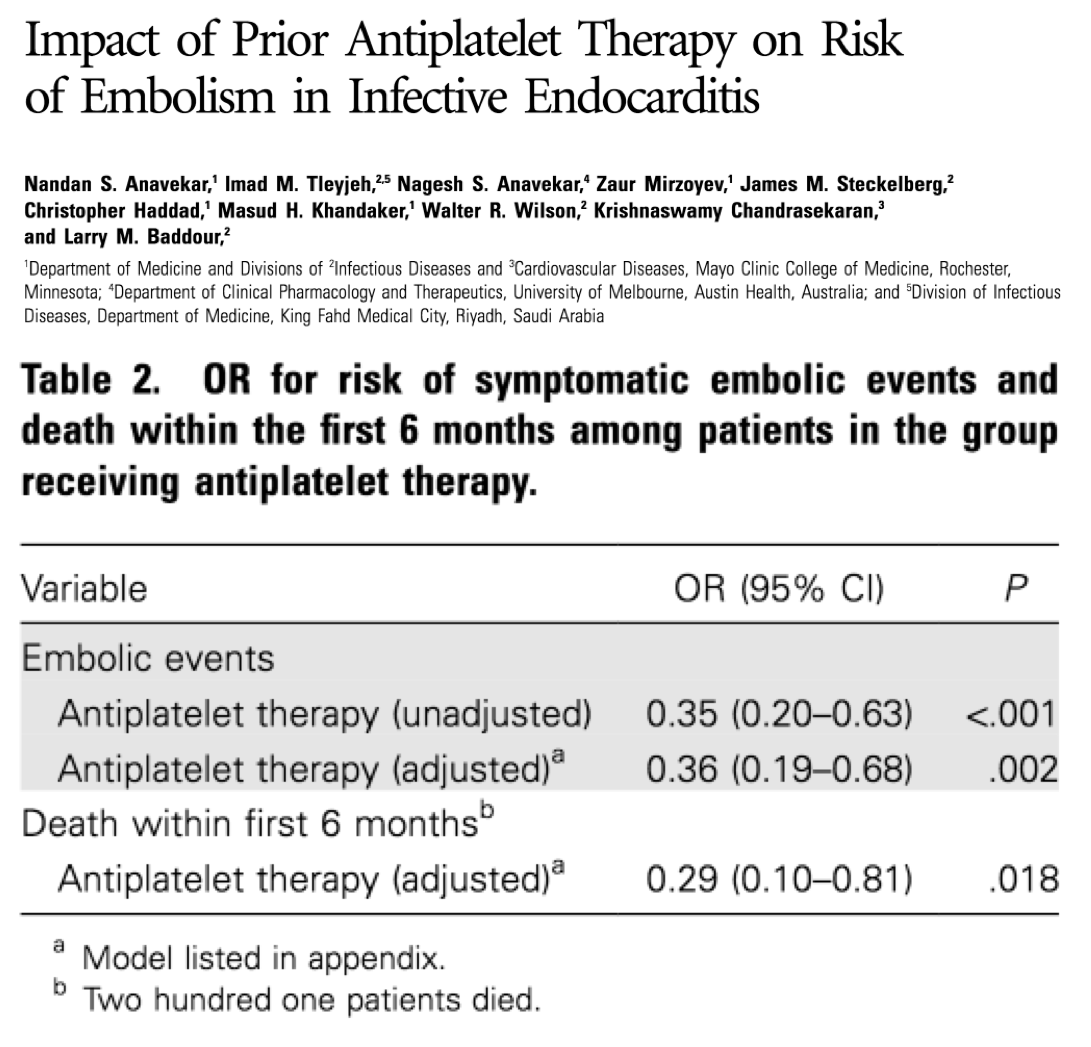
There is some evidence suggesting that antiplatelets might reduce the risk of IE (PMID 17407036; Pic).
That said, the data is not conclusive and the use of antiplatelets and/or anticoagulants for the prevention or treatment is not recommended.
https://www.ncbi.nlm.nih.gov/pubmed/21932963 ">https://www.ncbi.nlm.nih.gov/pubmed/21...
There is some evidence suggesting that antiplatelets might reduce the risk of IE (PMID 17407036; Pic).
That said, the data is not conclusive and the use of antiplatelets and/or anticoagulants for the prevention or treatment is not recommended.
https://www.ncbi.nlm.nih.gov/pubmed/21932963 ">https://www.ncbi.nlm.nih.gov/pubmed/21...
12/
With the pathogenesis of IE covered, we can now address the original question. Let& #39;s confirm that the tricuspid valve is more commonly involved in those with IVDU. One study found:
68% tricuspid
7% aortic
6% mitral
1% pulmonic
https://www.ncbi.nlm.nih.gov/pubmed/12866981 ">https://www.ncbi.nlm.nih.gov/pubmed/12...
With the pathogenesis of IE covered, we can now address the original question. Let& #39;s confirm that the tricuspid valve is more commonly involved in those with IVDU. One study found:
68% tricuspid
7% aortic
6% mitral
1% pulmonic
https://www.ncbi.nlm.nih.gov/pubmed/12866981 ">https://www.ncbi.nlm.nih.gov/pubmed/12...
13/
Why this difference? The tricuspid valve (TV) has lower shear stress. And, again, bacteria enter the venous system in most situations (i.e., they "see the TV first").
What makes the TV more vulnerable in those with IV drug use?
Why this difference? The tricuspid valve (TV) has lower shear stress. And, again, bacteria enter the venous system in most situations (i.e., they "see the TV first").
What makes the TV more vulnerable in those with IV drug use?
14/
There are surely multiple factors, but endothelial injury to the tricuspid valve is likely a key event. And what causes this injury?
Particulate matter that comes with the injected material.
http://www.ncbi.nlm.nih.gov/pubmed/116317 ">https://www.ncbi.nlm.nih.gov/pubmed/11...
There are surely multiple factors, but endothelial injury to the tricuspid valve is likely a key event. And what causes this injury?
Particulate matter that comes with the injected material.
http://www.ncbi.nlm.nih.gov/pubmed/116317 ">https://www.ncbi.nlm.nih.gov/pubmed/11...
15/
Interestingly, particulate matter >8-10 μm may not be able to pass through pulmonary capillaries, potentially "protecting" the aortic and pulmonic valves from this form of endothelial injury.
https://www.ncbi.nlm.nih.gov/pubmed/2197312 ">https://www.ncbi.nlm.nih.gov/pubmed/21...
Interestingly, particulate matter >8-10 μm may not be able to pass through pulmonary capillaries, potentially "protecting" the aortic and pulmonic valves from this form of endothelial injury.
https://www.ncbi.nlm.nih.gov/pubmed/2197312 ">https://www.ncbi.nlm.nih.gov/pubmed/21...
16/
There are many other factors that play a role in TV endocarditis, including:
*physiologic effects of injected substances (particularly cocaine)
*organism-specific factors (particularly S aureus)
*immune status
*bacterial load
https://www.ncbi.nlm.nih.gov/pubmed/10671344 ">https://www.ncbi.nlm.nih.gov/pubmed/10...
There are many other factors that play a role in TV endocarditis, including:
*physiologic effects of injected substances (particularly cocaine)
*organism-specific factors (particularly S aureus)
*immune status
*bacterial load
https://www.ncbi.nlm.nih.gov/pubmed/10671344 ">https://www.ncbi.nlm.nih.gov/pubmed/10...
17/
Before summing up, let& #39;s re-ask the original question.
Which of the following confers the greatest risk of infective endocarditis?
Before summing up, let& #39;s re-ask the original question.
Which of the following confers the greatest risk of infective endocarditis?
18/
Summary:
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Medium star" aria-label="Emoji: Medium star">IE occurs after endothelial injury, thrombus formation, and bacterial infection of thrombus
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Medium star" aria-label="Emoji: Medium star">IE occurs after endothelial injury, thrombus formation, and bacterial infection of thrombus
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Medium star" aria-label="Emoji: Medium star">In non-IVDU, the hemodynamics of the left heart predispose to IE
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Medium star" aria-label="Emoji: Medium star">In non-IVDU, the hemodynamics of the left heart predispose to IE
 https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Medium star" aria-label="Emoji: Medium star">In IVDU, particulate matter leads to TV endothelial injury and IE (among other factors!)
https://abs.twimg.com/emoji/v2/... draggable="false" alt="⭐️" title="Medium star" aria-label="Emoji: Medium star">In IVDU, particulate matter leads to TV endothelial injury and IE (among other factors!)
Summary:

 Read on Twitter
Read on Twitter
 platelet activation*S aureus production of coagulase which converts fibrinogen to fibrin https://www.ncbi.nlm.nih.gov/pubmed/21..." title="7/The result of endothelial injury is activation of the clotting cascade and creation of thrombus. Other factors fuel thrombus formation:*high shear stress https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> platelet activation*S aureus production of coagulase which converts fibrinogen to fibrin https://www.ncbi.nlm.nih.gov/pubmed/21..." class="img-responsive" style="max-width:100%;"/>
platelet activation*S aureus production of coagulase which converts fibrinogen to fibrin https://www.ncbi.nlm.nih.gov/pubmed/21..." title="7/The result of endothelial injury is activation of the clotting cascade and creation of thrombus. Other factors fuel thrombus formation:*high shear stress https://abs.twimg.com/emoji/v2/... draggable="false" alt="➡️" title="Rightwards arrow" aria-label="Emoji: Rightwards arrow"> platelet activation*S aureus production of coagulase which converts fibrinogen to fibrin https://www.ncbi.nlm.nih.gov/pubmed/21..." class="img-responsive" style="max-width:100%;"/>