1/
As #COVID19 runs rampant, many in #dermatology are being redeployed. In hopes of helping out, a #tweetorial:
CARING FOR THE #COVID PATIENT: A PRIMER FOR THE NONINTERNIST
#MedEd #FOAMEd #dermtwitter #medtwitter
Just for funsies: When was the last time you used a stethoscope?
As #COVID19 runs rampant, many in #dermatology are being redeployed. In hopes of helping out, a #tweetorial:
CARING FOR THE #COVID PATIENT: A PRIMER FOR THE NONINTERNIST
#MedEd #FOAMEd #dermtwitter #medtwitter
Just for funsies: When was the last time you used a stethoscope?
2/
 caveats
caveats
 When treating your patients, abide by your institutional policies and treat the person in front of you. These tweets are just some personal musings & NOT medical advice.
When treating your patients, abide by your institutional policies and treat the person in front of you. These tweets are just some personal musings & NOT medical advice.
 The understanding we have of #COVID is always changing, so be vigilant about new info!
The understanding we have of #COVID is always changing, so be vigilant about new info!
 caveats
caveats
 When treating your patients, abide by your institutional policies and treat the person in front of you. These tweets are just some personal musings & NOT medical advice.
When treating your patients, abide by your institutional policies and treat the person in front of you. These tweets are just some personal musings & NOT medical advice. The understanding we have of #COVID is always changing, so be vigilant about new info!
The understanding we have of #COVID is always changing, so be vigilant about new info!
3/
Before we get to specifics re: #COVID19, some general advice.
Tip: When in doubt, ASK. No one is expecting you to know everything. This is new for you and folks will be thankful for your presence & assistance! The nurses & other physicians are a treasure trove of information.
Before we get to specifics re: #COVID19, some general advice.
Tip: When in doubt, ASK. No one is expecting you to know everything. This is new for you and folks will be thankful for your presence & assistance! The nurses & other physicians are a treasure trove of information.
4/
Tip: You’re an internist now! You care about ALL organs. Every single complaint or lab abnormality is a potential problem to address.
I like to keep a running list of problems, & then when writing my note, decide what can be lumped together, deferred, and what needs a plan.
Tip: You’re an internist now! You care about ALL organs. Every single complaint or lab abnormality is a potential problem to address.
I like to keep a running list of problems, & then when writing my note, decide what can be lumped together, deferred, and what needs a plan.
5/
Tip: You might be coming from the ambulatory side, so remember, not all issues need to be fixed. Focus on the inpatient ones; outpatient issues can be left for after discharge.
So if you see a BCC, as much as you want to biopsy, leave it for later. You’re an internist now!
Tip: You might be coming from the ambulatory side, so remember, not all issues need to be fixed. Focus on the inpatient ones; outpatient issues can be left for after discharge.
So if you see a BCC, as much as you want to biopsy, leave it for later. You’re an internist now!
6/
Okay, let’s talk #COVID19.
While the respiratory issues are what lands the patient in the hospital, it’s a multiorgan system disease affecting much more than the lungs.
I thought this website was a nice way to see them all laid out with citations:
https://bestpractice.bmj.com/topics/en-us/3000168/complications
Okay, let’s talk #COVID19.
While the respiratory issues are what lands the patient in the hospital, it’s a multiorgan system disease affecting much more than the lungs.
I thought this website was a nice way to see them all laid out with citations:
https://bestpractice.bmj.com/topics/en-us/3000168/complications
7/
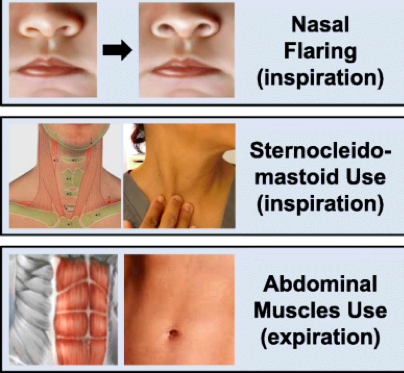
So things to always be vigilant about:
Your patient’s oxygenation (O2 sat)
Their work of breathing (are they getting tired? see pic!)
Hemodynamics (BP, HR)
Rashes/labs that could mean thrombosis
And ALWAYS listen to your nurses. If they’re worried, you should be too.
So things to always be vigilant about:
Your patient’s oxygenation (O2 sat)
Their work of breathing (are they getting tired? see pic!)
Hemodynamics (BP, HR)
Rashes/labs that could mean thrombosis
And ALWAYS listen to your nurses. If they’re worried, you should be too.
8/
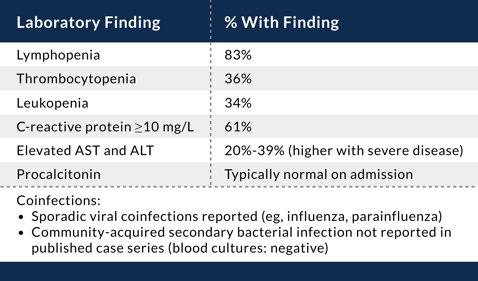
LABS: We’ve seen that COVID patients get some typical lab abnormalities. Namely:
Lymphopenia
Elevated ALT/AST
You may need to do a cursory work up for this, but if that’s negative, it may just be COVID. Other labs may imply severe disease, but I’ll leave that to the experts.
LABS: We’ve seen that COVID patients get some typical lab abnormalities. Namely:
Lymphopenia
Elevated ALT/AST
You may need to do a cursory work up for this, but if that’s negative, it may just be COVID. Other labs may imply severe disease, but I’ll leave that to the experts.
9/
Let's talk LUNGS: While it may have been years since you’ve used a , don’t fret. No matter what you hear on your exam, the O2 Sat (+/- imaging) will likely drive most of your decision making.
, don’t fret. No matter what you hear on your exam, the O2 Sat (+/- imaging) will likely drive most of your decision making.
Track O2 use and how that changes over time. Also whether they are getting tired!
Let's talk LUNGS: While it may have been years since you’ve used a
 , don’t fret. No matter what you hear on your exam, the O2 Sat (+/- imaging) will likely drive most of your decision making.
, don’t fret. No matter what you hear on your exam, the O2 Sat (+/- imaging) will likely drive most of your decision making. Track O2 use and how that changes over time. Also whether they are getting tired!
10/
What should you do for a worsening respiratory status? Past nasal cannula, don’t forget you can use:
Non-rebreather
High flow O2
Ask your team & respiratory therapy about options prior to mechanical ventilation.
 Caution with nebulizers
Caution with nebulizers They can aerosolize the virus!
They can aerosolize the virus!
What should you do for a worsening respiratory status? Past nasal cannula, don’t forget you can use:
Non-rebreather
High flow O2
Ask your team & respiratory therapy about options prior to mechanical ventilation.
 Caution with nebulizers
Caution with nebulizers They can aerosolize the virus!
They can aerosolize the virus!
11/
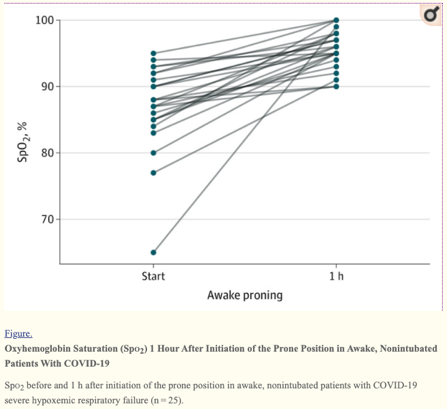
Aside from delivering O2 in a new way, don’t forget about PRONING! Remember V/Q mismatch? This is a non-invasive way to address that problem by having your patient lie on their belly (see pic 1).
Check out the impressive results from an early publication (in pic 2)!
Aside from delivering O2 in a new way, don’t forget about PRONING! Remember V/Q mismatch? This is a non-invasive way to address that problem by having your patient lie on their belly (see pic 1).
Check out the impressive results from an early publication (in pic 2)!
12/
What about meds for COVID? First, follow your institution’s guidelines as many have trials available and have protocolized a lot.
Remedesivir is suggested for hospitalized patients as it has been shown to potentially shorten recovery time. Caution with ALT/AST and BUN/Cr.
ALT/AST and BUN/Cr.
What about meds for COVID? First, follow your institution’s guidelines as many have trials available and have protocolized a lot.
Remedesivir is suggested for hospitalized patients as it has been shown to potentially shorten recovery time. Caution with
 ALT/AST and BUN/Cr.
ALT/AST and BUN/Cr.
13/
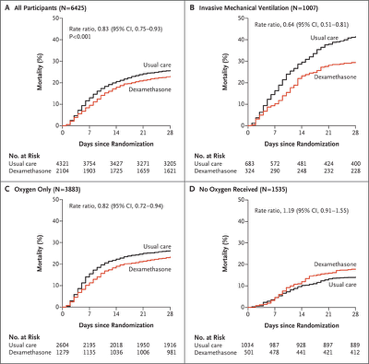
Dexamethasone has good evidence for benefit in HYPOXEMIC COVID patients. But as you give systemic steroids, watch the following:
blood sugars
Blood pressures
Mental status changes
Drug-drug interactions (it’s a CYP3A4 inducer)
Check out those KM-curves from RECOVERY trial!
Dexamethasone has good evidence for benefit in HYPOXEMIC COVID patients. But as you give systemic steroids, watch the following:
blood sugars
Blood pressures
Mental status changes
Drug-drug interactions (it’s a CYP3A4 inducer)
Check out those KM-curves from RECOVERY trial!
14/
What about non-respiratory issues?
1) DVT prophylaxis is SUPER important since COVID can thrombosis!
thrombosis!
2) Have a low threshold for bacterial processes too. COVID patients can have non-COVID issues, so if worried, consider antibiotics or even checking procalcitonin upfront.
What about non-respiratory issues?
1) DVT prophylaxis is SUPER important since COVID can
 thrombosis!
thrombosis!2) Have a low threshold for bacterial processes too. COVID patients can have non-COVID issues, so if worried, consider antibiotics or even checking procalcitonin upfront.
15/
When should you start to think about ICU transfer?
Hypoxia/Hypoxemia
Increased work of breathing (patient tiring out)
Altered mental status
Hemodynamic instability
Given the way things are looking right now, fingers crossed a bed is available in the unit if you need it!
When should you start to think about ICU transfer?
Hypoxia/Hypoxemia
Increased work of breathing (patient tiring out)
Altered mental status
Hemodynamic instability
Given the way things are looking right now, fingers crossed a bed is available in the unit if you need it!
16/
Some other basic IM tips:
 Pain? Start with round the clock acetaminophen.
Pain? Start with round the clock acetaminophen.
 Don’t give maintenance IVF.
Don’t give maintenance IVF.
 Docusate doesn’t do anything.
Docusate doesn’t do anything.
 If you forgot a lab, try to add it onto your morning labs first.
If you forgot a lab, try to add it onto your morning labs first.
 Be organized, use checkboxes!
Be organized, use checkboxes!
 When in doubt – ask a nurse!
When in doubt – ask a nurse!
Some other basic IM tips:
 Pain? Start with round the clock acetaminophen.
Pain? Start with round the clock acetaminophen. Don’t give maintenance IVF.
Don’t give maintenance IVF.  Docusate doesn’t do anything.
Docusate doesn’t do anything. If you forgot a lab, try to add it onto your morning labs first.
If you forgot a lab, try to add it onto your morning labs first. Be organized, use checkboxes!
Be organized, use checkboxes! When in doubt – ask a nurse!
When in doubt – ask a nurse!
17/
But what about protecting yourself? Let’s start by saying:
PPE WORKS
But you have to use it correctly. So double check before entering any COVID patient’s room. If using an N95, make sure you do a quick fit-check and don/doff properly!
But what about protecting yourself? Let’s start by saying:
PPE WORKS
But you have to use it correctly. So double check before entering any COVID patient’s room. If using an N95, make sure you do a quick fit-check and don/doff properly!
18/
Let’s talk wellness. Caring for #COVID19 patients can be overwhelming, depressing, and all-consuming.
Our colleagues have been doing this nonstop, so we should not only thank them, but also listen to them as they’ll have plenty of coping strategies to share!
Let’s talk wellness. Caring for #COVID19 patients can be overwhelming, depressing, and all-consuming.
Our colleagues have been doing this nonstop, so we should not only thank them, but also listen to them as they’ll have plenty of coping strategies to share!
19/
I hope this helps some of you feel more comfortable on #COVID19 teams!
A HUGE thank you to @AvrahamCooperMD for helping me vet this #tweetorial, & a standing invitation to #medtwitter to add other tips for your redeployed colleagues!
for your redeployed colleagues!
Good luck, stay safe, & you got this!
I hope this helps some of you feel more comfortable on #COVID19 teams!
A HUGE thank you to @AvrahamCooperMD for helping me vet this #tweetorial, & a standing invitation to #medtwitter to add other tips
 for your redeployed colleagues!
for your redeployed colleagues!Good luck, stay safe, & you got this!

 Read on Twitter
Read on Twitter