This study found that Epstein Barr #Virus (EBV) IgM antibody seropositive #COVID-19 patients had a 3.09-fold increased risk of fever compared to EBV seronegative patients. Inflammatory markers like C-reactive protein were also higher in the EBV+ patients: https://www.researchsquare.com/article/rs-21580/v1">https://www.researchsquare.com/article/r...
2/ The study is a small, but good example of the how already-acquired persistent #pathogens can influence how a person responds to a new #infection: the existing pathogen(s) might cause additional symptoms or influence how the #immune system can respond to the new infection
3/ For example this study found that persistent Cytomegalovirus (CMV) infection caused ~10% of all T cells in CMV+ individuals to be directed against that virus. Could harboring CMV then change how the adaptive immune system responds to COVID-19?: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4302727/">https://www.ncbi.nlm.nih.gov/pmc/artic...
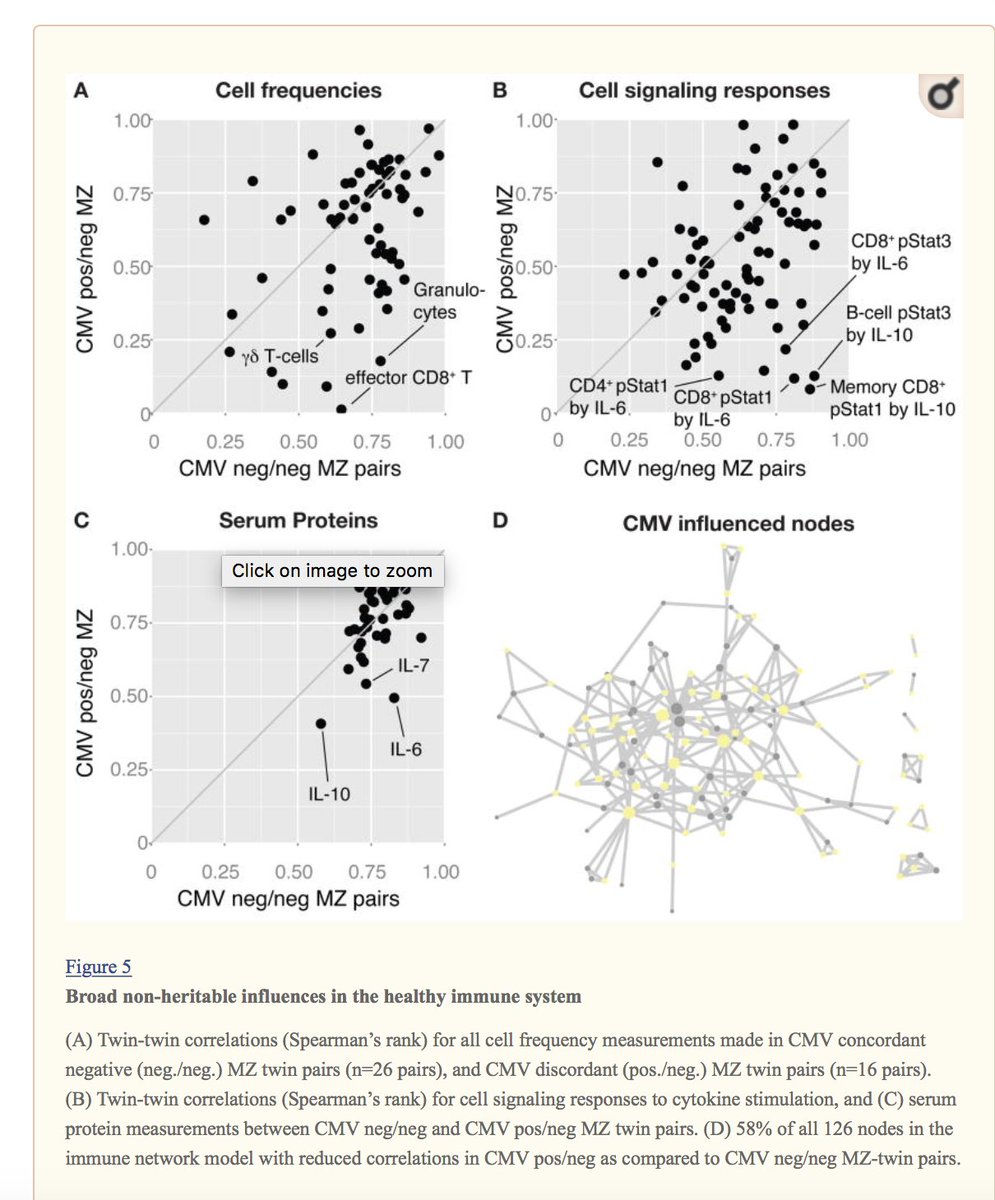
4/ The same team also measured how having #CMV impacted subjects’ immune cell frequencies, cell signaling responses, and serum protein levels: all factors that significantly impact how the immune system can respond to a new infection
5/ They found that CMV modulated the above immune parameters so extensively that having the virus impacted 119 of all 204 measurements (58%)! This illustrated “how at least one type of microbial exposure can dramatically modulate the overall immune profile of healthy individuals”
6/ A simple terms summary is the above study is that: if two people are exposed to COVID-19, and one harbors CMV and the other doesn’t, the immune response to COVID-19 will inevitably differ between the two people, which might impact COVID-19 severity
7/ Then, think about the many other persistent pathogens people often harbor - related # #herpesviruses, mycobacteria, #Borrelia etc. All these pathogens also dramatically modulate the immune response…how does that play out with new infections like COVID-19??
8/ The topic is important b/c we tend to think of predisposition for disease as pertaining only to the human #genome (eg: what gene variants might a patient have that cld influence how the immune system manages a new #infection/exposure?)
9/ But the persistent #pathogens a patient already harbors at the time of a new infection like #COVID-19 are also MAJOR sources of “predisposition” that shape the immune response and the gene expression of infected cells
10/ The trend is also key in chronic conditions tied to infection like ME/CFS: in #MECFS, are people who already harbor one serious pathogen (like EBV) more likely to develop chronic symptoms when exposed to another serious pathogen (like an #enterovirus)?? etc, etc. etc

 Read on Twitter
Read on Twitter